A CPAP device can immensely affect your life if you have asthma and obstructive sleep apnea (OSA).
In this comprehensive guide on asthma and sleep apnea, we will explore the connection between these two respiratory disorders, delving into the role inflammation plays in OSA among asthmatic patients and identifying common symptoms that could indicate its presence.
Also, we’ll talk about how to use a CPAP machine for optimal comfort and relief from OSA-related issues.

In addition to addressing potential side effects of using a CPAP device, such as dryness or mask irritation, we’ll examine whether these machines may help prevent nighttime asthma attacks based on existing research findings.
Finally, you’ll learn about consulting your doctor if you suspect sleep apnea affects your quality of life alongside your asthma condition.
Join us as we uncover valuable insights into managing asthma and sleep apnea symptoms through CPAP therapy and explore practical tips to enhance your well-being.
The Connection Between Asthma and Obstructive Sleep Apnea
As highlighted in a 2009 study published in the Journal of Clinical Sleep Medicine, sleep apnea and asthma can affect each other, making both conditions worse.
Before we dive into the details, let’s look at a brief overview of each condition.
- Sleep apnea is a sleep disorder where a person’s breathing is repeatedly interrupted during sleep, leading to poor sleep and less oxygen in the blood.
- Asthma is when a person’s airways become narrow and inflamed, causing difficulty breathing, coughing, and wheezing.
When someone has sleep apnea, their airways can become more inflamed, worsening asthma symptoms.
Sleep apnea can also lead to gastroesophageal reflux disease (GERD)—you might know it as acid reflux.
This can make breathing difficult and increase asthma attack frequency during sleep.
Looking at the relationship from the opposite direction, asthma can worsen sleep apnea by causing more inflammation in your airways.
This can make breathing harder and reduce the benefits of positive airway pressure therapy while sleeping.
Some medicines used to treat asthma, like steroids, can cause weight gain, a risk factor for sleep apnea.
Sleep apnea can be a significant health hazard when coupled with severe asthma, so understanding the link between them is critical to maintaining good overall well-being.
Let’s look at some specific interactions that might help you make more informed decisions with the help of your sleep specialist, respiratory therapist, or primary care provider.
How Inflammation Complicates Symptoms when Dealing with OSA and Asthma
When asthma-related inflammation is present, it can narrow your airways, making it more likely for them to become blocked or collapse during sleep.
This can lead to the onset of sleep apnea symptoms or worsen existing sleep apnea symptoms, causing more frequent and prolonged pauses in breathing while you sleep.
This is particularly relevant for more aggressive forms of the condition, such as neutrophilic asthma.
These breathing interruptions can result in sleep fragmentation, daytime fatigue, and an increased risk of other health issues, such as high blood pressure or heart disease.

Likewise, when your airway is blocked during sleep apnea episodes, the body’s natural response is to force the airway open.
This can increase pressure in the chest and throat, causing further inflammation and irritation.
The inflammation can then affect the airways in the lungs, making them more sensitive and prone to constriction—a common characteristic of asthma.
Furthermore, the low oxygen levels associated with sleep apnea can also cause the body to release certain chemicals that promote inflammation.
This increased inflammation can worsen existing asthma symptoms, making it harder to manage the condition effectively.
GERD, Asthma, and Sleep Apnea: A Trio of Night Time Discomfort
Gastroesophageal reflux disease (GERD) occurs when stomach acid flows back into the esophagus (food pipe) due to a weak or dysfunctional lower esophageal sphincter.
You likely know acid reflux can cause heartburn, chest pain, sleep fragmentation, and other uncomfortable symptoms.
But did you know there is a connection between GERD and nighttime asthma attacks?
A 2001 study published in the American Journal of Medicine found “a significant correlation between lower respiratory resistances and spontaneous GER.”

When you lie down, it’s easier for the stomach acid to flow back up into your esophagus.
If the acid reaches your throat, it may be inhaled into the lungs, causing irritation and inflammation of the airways.
This inflammation can trigger an asthma attack or worsen existing asthma symptoms.
Acid reflux can also trigger a condition known as reflex bronchoconstriction, in which stimulation nerves in the esophagus can cause airways in your lungs to constrict.
Neither issue is ideal for people with sleep apnea, asthma, and other respiratory disorders, as both make breathing even harder.
The Interplay Between Asthma Treatments and Sleep Apnea
A 2019 study published in the American Journal of Respiratory and Critical Care Management found a correlation between the long-term use of inhaled corticosteroids—a standard treatment for severe asthma symptoms—and collapse of the upper airways during sleep—a leading cause of obstructive sleep apnea.
This follows a 2015 study published in PLOS ONE, which cites a 33% increase in the adjusted hazard ratio for people developing sleep apnea symptoms when receiving inhaled steroid treatments for their asthma symptoms vs those who did not.
An adjusted hazard ratio in a medical study is a measure used to compare the likelihood of a specific event (such as a health issue or treatment outcome) occurring in two different groups of people over a period of time, with the term “adjusted” meaning that the researchers have considered other factors that might influence the results, such as age, gender, other health conditions, and lifestyle.
While this doesn’t mean you should forego treatment of your asthma symptoms—especially if you have acute or severe asthma symptoms—it is essential to know that the relationship between these two common respiratory conditions works both ways.
Identifying Symptoms of Obstructive Sleep Apnea in Asthmatics
Fortunately, while many of the ways in which sleep apnea and asthma interact are complex, the symptoms of asthmatic patients compared almost identically to those without asthma.
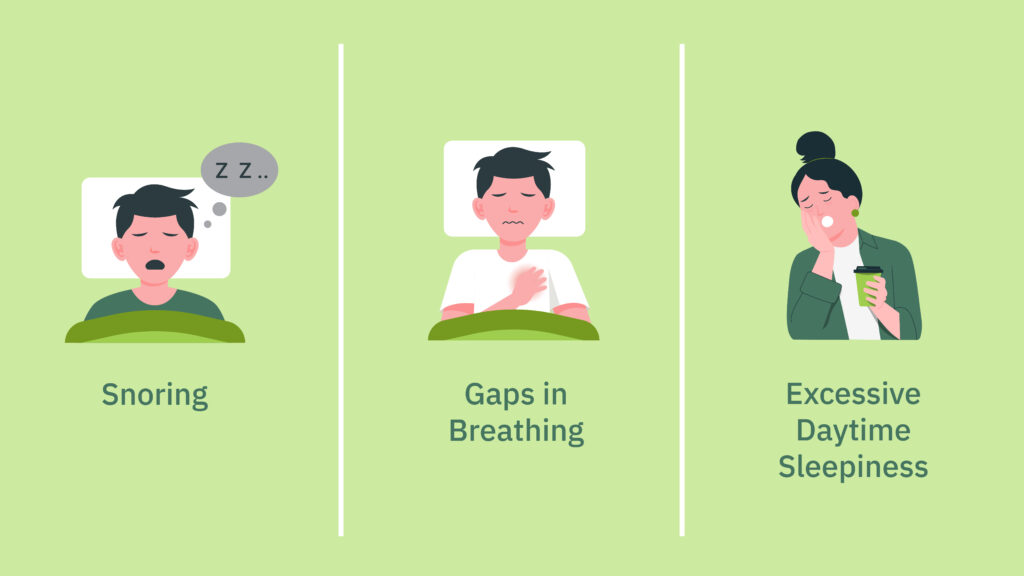
If you’re unsure what to look for when determining if you should consult a healthcare professional, look for the following three symptoms:
- Snoring: Snoring is often one of the first signs that someone may have obstructive sleep apnea. While not all snorers have sleep apnea, it’s essential for those with asthma who snore loudly or frequently to consult a healthcare professional about potential risks as this could indicate deformation or collapse of upper airways.
- Gaps in Breathing: If you or your partner notice pauses in your breath while sleeping followed by gasping or choking sounds when you start breathing again, this could indicate that you’re experiencing episodes related to obstructive sleep apnea. This can be trickier to catch for those with severe asthma, as waking up gasping or choking might be mistaken for an asthma attack. If you notice frequent nighttime asthma attacks, monitoring your respiratory rates before the attack might provide additional insights to bring up with your primary care provider or respiratory specialist.
- Excessive Daytime Sleepiness: Consistently feeling tired or sleepy during the day despite getting a whole night’s rest can be another symptom of sleep apnea. This is because your body isn’t receiving adequate oxygen levels throughout the night—a condition known as intermittent hypoxia—due to interrupted breathing patterns. These interruptions can also lead to sleep fragmentation, lowering overall sleep quality—even if you don’t remember waking up during the night.
If you have asthma and are experiencing any of these symptoms, discussing them with your healthcare provider is crucial.
They can determine whether an evaluation for obstructive sleep apnea is necessary and if a CPAP machine is beneficial in managing both conditions.
Using CPAP Machines for Asthma Patients with Sleep Apnea
Continuous positive airway pressure (CPAP) therapy is primarily used to treat obstructive sleep apnea.
However, according to a 2007 study published in the European Respiratory Journal, people with asthma who have sleep apnea can benefit from using a CPAP machine.
Maintaining constant airflow through the respiratory system reduces snoring and other symptoms associated with sleep apnea that could exacerbate asthma symptoms.
A CPAP machine delivers continuous pressurized air into the user’s airways, preventing them from collapsing during sleep and maintaining steady breathing patterns throughout the night.
This consistent oxygen flow alleviates sleep apnea symptoms and may also help address asthma symptoms for individuals with asthma and sleep apnea.
Potential benefits include:
- Reduced snoring: By keeping airways open, CPAP use minimizes snoring, which is common in sleep apnea and can trigger asthma symptoms.
- Improved oxygen levels: Better airflow due to CPAP use ensures adequate oxygen levels, helping to alleviate asthma symptoms during sleep.
- Enhanced sleep quality: CPAP use leads to fewer nighttime awakenings, allowing for more restful sleep and benefiting both sleep apnea and people with asthma.
- Reduced inflammation: By maintaining open airways, CPAP use reduces inflammation, which can improve both sleep apnea and asthma symptoms.
Choosing the Right Type of Mask for Optimal Comfort
Finding a comfortable mask is crucial when starting your journey towards better sleep quality through CPAP therapy.
There are several types of masks available to suit different preferences:
- Nasal pillows: These small cushions fit directly into each nostril and provide minimal contact with your face.
- Nasal masks: Covering just your nose, these masks form a seal around its base to deliver pressurized air effectively.
- Full-face masks: Ideal for mouth breathers or those who experience nasal congestion at night, full-face masks cover both your nose and mouth while providing an airtight seal.
Try different mask styles and sizes to find the one that best fits your face shape and offers maximum comfort.
A proper fit ensures optimal CPAP therapy effectiveness while minimizing potential side effects such as skin irritation or feelings of claustrophobia.
If you’re unsure which type of mask is right for you, you can check our guide, “The Best CPAP Mask Types for Every Type of Sleeper (Mask Types Compared),” for an easy-to-understand overview of the pros and cons of various mask types—including recommendations from top models on the market today.
If you’re unsure afterward, consult a sleep specialist or CPAP supply store.
They can help guide you in making an informed decision based on your needs and preferences.
Minimizing Potential Side Effects When Using a CPAP Machine
While many patients experience relief from their sleep apnea after starting continuous positive airway pressure therapy, there are potential side effects you should be aware of when using a CPAP machine.
Some common complaints include dry mouth or nose, skin irritation around the mask area, or feelings of claustrophobia while wearing the device.
This section will discuss ways to address these discomforts and tips for finding comfortable masks that minimize irritation.
Addressing Dryness and Soreness with Humidification
If you’re experiencing dryness in your mouth or nose, sore throat or nasal passages, frequent nosebleeds, or sinus discomfort due to CPAP therapy, consider using the humidifier on your device.
A heated humidifier often alleviates these symptoms by adding moisture to the air you breathe during treatment.
Many modern CPAP machines come with built-in humidifiers. However, standalone options are also available if yours does not include one.
Remember, if you use the humidifier, clean the humidification chamber regularly to avoid unwanted smells and prevent bacterial growth or allergen build-up.
You can find out more in our guide on CPAP machine cleaning & maintenance fundamentals.
Tips on Finding Comfortable Masks That Minimize Skin Irritation and Discomfort
While CPAP masks have come a long way in terms of both functionality and comfort, they’re still not a one-size-fits-all solution.
However, each manufacturer offers an array of mask designs—often with individual sizes for each model—to help you find a comfortable and secure fit.
If you’re not sure where to start or are experiencing discomfort with your existing mask, these tips should help.
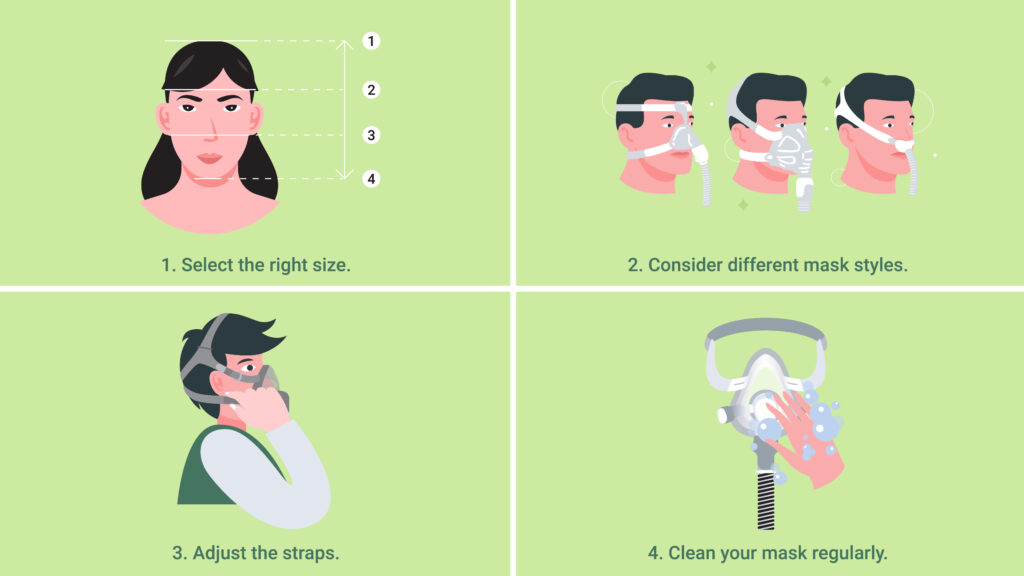
- Select the right size: Choosing a mask that fits properly is crucial for comfort and effectiveness. Measure your face according to manufacturer guidelines and select an appropriate size based on those measurements.
- Consider different mask styles: As discussed above, various types of masks are available for use with CPAP machines. Try different styles until you find one that fits comfortably and securely. Smaller mask formats can help if you experience claustrophobia when wearing your CPAP mask or are looking for options that won’t obstruct your vision.
- Adjust the straps: Ensure your headgear is adjusted correctly to provide a secure fit without causing discomfort or pressure sores. The ideal fit is tight enough to maintain a seal but not so tight that it squeezes your head. If you’re experiencing skin irritation, strap covers made from soft fabric can also help.
- Clean your mask regularly: Keeping your mask clean is essential for hygiene and comfort. Follow the manufacturer’s instructions on cleaning and maintenance of your specific CPAP mask model. Periodically washing the cushion can help prevent skin irritation caused by dirt or oil build-up.
These tips are just the basics.
However, incorporating them into your daily routine may help alleviate some common side effects of using a CPAP machine, ultimately improving overall treatment experience and effectiveness.
Always consult with your healthcare provider if you experience extended discomfort or have concerns about potential side effects related to CPAP therapy.
Looking for more information on this topic?
Check out our full guide, “CPAP Machine Use Essentials: Proper Mask Fitment and Other Critical Considerations.”
Conclusion
Asthma and sleep apnea are both conditions that can significantly impact a person’s quality of life.
If you think your asthma might be accompanied by sleep apnea, speak to a doctor about your sleep study options.
We have guides on both at-home sleep studies and laboratory-based sleep studies if you need help determining what to expect.
If diagnosed with sleep apnea, a CPAP machine can help alleviate symptoms like snoring, interrupted breathing during sleep, and excessive daytime sleepiness.
While these devices are not a primary method to treat asthma and cannot help to resolve the symptoms of already-occurring asthma attacks, growing evidence shows that CPAP machines can improve the quality of life for asthmatic patients compared to those with untreated sleep apnea.
While there may be some initial discomfort when starting CPAP therapy, finding the right mask fit and adding accessories like humidifiers can make the experience more comfortable.
If you or someone you love suffers from sleep apnea, then CPAP Supply has the solution. We offer new and refurbished CPAP machines that provide an effective and affordable way to treat this common disorder. With our top-of-the-line products and expert customer service, we can help improve your quality of life with a reliable therapy system explicitly tailored to your needs. Don’t wait any longer—take control of your health today by getting the relief you deserve!

