Why you might consider an at-home sleep study and what to expect during the process

It wasn’t long ago that diagnosing sleep apnea required spending a night (or more) in a sleep lab while connected to an array of medical equipment—as if falling asleep in a strange bed wasn’t already hard enough.
Today, at-home sleep studies—also known as home sleep apnea tests or HSTs—offer a convenient, affordable, and far more comfortable alternative to lab-based tests when diagnosing obstructive sleep apnea.
Availability will depend on your province. Currently Alberta, British Columbia, New Brunswick, and Quebec allow home sleep studies while Ontario requires lab-based sleep studies instead.
If you’re considering an at-home sleep apnea test—or are looking for more on what to expect at an upcoming test—this guide will explore how to obtain an at-home sleep study, how most sleep studies work, what you can expect, and some best practices to help improve the chances of gathering the data your doctor needs.
Note: While this guide can give you an idea of what to expect from an at-home sleep study, it is important to discuss your symptoms with your CPAP supplier, primary care provider, or sleep specialist to understand the best options for your specific needs.
Obtaining An At-Home Sleep Study
Before we dive into what to expect, it’s important to discuss exactly how you can get an at-home sleep study in the first place.
These aren’t over-the-counter devices or something you can pick up at the local health store. And even if you find one to purchase, you’d still need someone to interpret the data gathered.
Instead, you’ll need a prescription—most likely from your family doctor or a sleep specialist. A prescription will provide access to the required equipment and ensure that someone will analyze the data gathered to help guide any apnea-related medical decisions needed.
While exact steps might vary based on local practices or the severity of your symptoms, the process will generally involve a handful of steps similar to those listed below.
Starting the Process
Everything starts with talking to a medical professional. They’ll discuss your sleep apnea symptoms, check for any potential complicating concerns, and rule out the possibility of other issues or sleep disorders.
If they suspect sleep apnea is the cause of your medical concerns, they might recommend a home sleep study.
Picking Up Your Home Sleep Study Equipment
In most cases, your care provider will prescribe a test and provide any equipment you need within the same visit. If they do not stock the equipment on-site, they’ll give you the information for a local supplier or facility where you can find everything you need.
Most health care providers will also provide a quick walkthrough of any instructions needed to perform the test.
The most commonly used option is the Type 3 Home Sleep Apnea Testing or HSAT device. However, you might also find that you are prescribed an Apnea Risk Evaluation System (ARES) or WatchPAT device instead.
Don’t worry though! While test options can vary slightly, they’re all fairly straightforward to use.
Performing Your At-Home Sleep Study
Once you have your equipment, carefully follow the instructions provided to be sure you gather accurate data for your physician or sleep specialist to analyze.
The length of time required can vary between 1 to 3 days. You won’t need to interact with the data or perform any complex operations. Just keep your equipment safe, and it will collect everything required!
Following Up on Your Home Sleep Test
Once you’ve collected the required data, return your equipment to your healthcare provider or sleep specialist. They’ll analyze the data and outline recommendations and options you might have to address your sleep apnea symptoms, including PAP therapy.
It’s important to note that while home sleep tests are accurate and dependable for detecting moderate to acute obstructive sleep apnea cases, they aren’t the best option for mild apnea cases or other sleep disorders, such as restless leg syndrome (RLS), periodic limb movements disorder (PLMD), or narcolepsy.
If your doctor still suspects sleep apnea—or believes another sleep disorder might be involved—after an at-home sleep test, they might request a more complex polysomnography (PSG) test—or lab-based sleep study—to confirm or deny their diagnosis.
Home Sleep Apnea Test Device Components and Their Functions
With the process broken down, let’s now dive into how the tests work. Since the Type 3 HSAT device is the most commonly used test, we’ll use it as our primary example.

The typical HSAT measures three physiological traits while you sleep:
- Breathing and airflow rates
- Nasal Pressure
- Blood oxygen levels
It does so using a few different components. While exact designs might vary slightly, most HSAT kits include:
- A chest strap or respiratory effort sensor belt: Helps to assess your respiratory effort by tracking the rise, expansion, and fall of your chest. It also serves as a secure, safe place for additional smaller components which might be easily lost or dislodged while sleeping.
- Nasal cannula: This plastic tube looks much like what you might find used for oxygen therapy with a thin, flexible body that loops over the ears and inserts into your nostrils. It is used to measure airflow as you breathe normally during your sleep.
- Pulse Oximeter: If you’ve ever been to the doctor and had them clamp a little box to the end of your finger as part of triage or check-in, it was probably a pulse oximeter. These tiny devices measure your blood’s oxygen saturation levels while you sleep. Certain models will also measure and record your heart rate to provide additional data to your physician.
Unlike a lab-based sleep study, these limited measurements mean that the HSAT devices can’t tell you much about your sleep. Instead, it focuses on your breathing. But by comparing the factors above, your physician or sleep specialist can identify apnea episodes, estimate how severe your sleep apnea symptoms are, and help to further your diagnosis.
The data from an at-home sleep apnea test is typically enough to start APAP treatment. It might also help to uncover the potential existence of other concerns which warrant further investigation. The next steps are likely to vary both by your results and any local requirements.
The Pros and Cons of At-Home Sleep Apnea Tests
With the how’s and what’s of at-home sleep apnea testing covered, let’s take a moment to look at why you might want an at-home test (and why you might not!)
Pros
- You can sleep in your own home and bed
- You can gather data on your schedule, not the schedule of a lab
- Home-based sleep apnea tests are often more simple
- At-home sleep apnea tests are more affordable than lab-based options
- Home-based tests provide better results for those with anxiety or trouble getting comfortable in new locations
- Accessible for the elderly, homebound, or those already receiving in-home healthcare services
Cons
- Only effective for diagnosing obstructive sleep apnea (OSA) and might miss other forms of sleep apnea
- Will not detect other sleeping disorders, including circadian rhythm disorders, insomnia, hypersomnia, narcolepsy, breathing disorders, periodic limb movement disorders (PLMD), or restless leg syndrome (RLS)
- They might fail to record data for mild sleep apnea cases
- Parts of the device might come off in your sleep, rendering data invalid
- Not available everywhere in Canada. For example, Ontario requires lab-based studies for most apnea diagnosis.
At-Home Sleep Apnea Test Best Practices
As mentioned above, your sleep specialist or physician will likely provide instructions on properly administering your at-home sleep apnea test. Exact steps might vary between test types.
However, the following tips offer a solid foundation for creating reliable test data while helping to minimize the discomfort you might experience while performing the test.
1. Don’t Nap On the Day of Your Test

While this might seem like common sense, daytime naps are a reasonably common habit—especially if you’ve experienced poor sleep quality due to apnea symptoms.
By making sure you’re tired and ready to sleep, you can avoid laying there feeling uncomfortable, reduce the risk of tossing and turning, and ensure that your sleep is deep enough to provide reliable data.
2. Skip the Mid-Day Coffee, Soda, or Tea

If you usually partake in a mid-day pick-me-up, skip it on your testing day. Caffeine can make it harder for you to fall asleep, alter the quality of your sleep, or make you more anxious and uncomfortable than you might be otherwise. In general, doctors recommend avoiding caffeine anytime after noon on the days you plan to gather data. If you absolutely must have your cup or two a day, make sure to plan your morning accordingly.
3. No Alcohol After Noon Either

From breathing rhythms and heart rate to brain patterns and mood, alcohol has wide-ranging effects on the human body and the systems which keep it running smoothly. Avoiding alcohol after noon on testing days ensures your HSAT can gather dependable data.
4. Stick to Your Routine

Unless otherwise directed, stick to your nightly routine as much as possible. Sleep where you’d typically sleep using the same pillows and sleepwear. Listen to the same music or play the TV if that is what suits you!
If you make yourself uncomfortable or change too many variables, it could lead to inaccuracies in your results!
5. Sleep On Your Side or Back If Possible
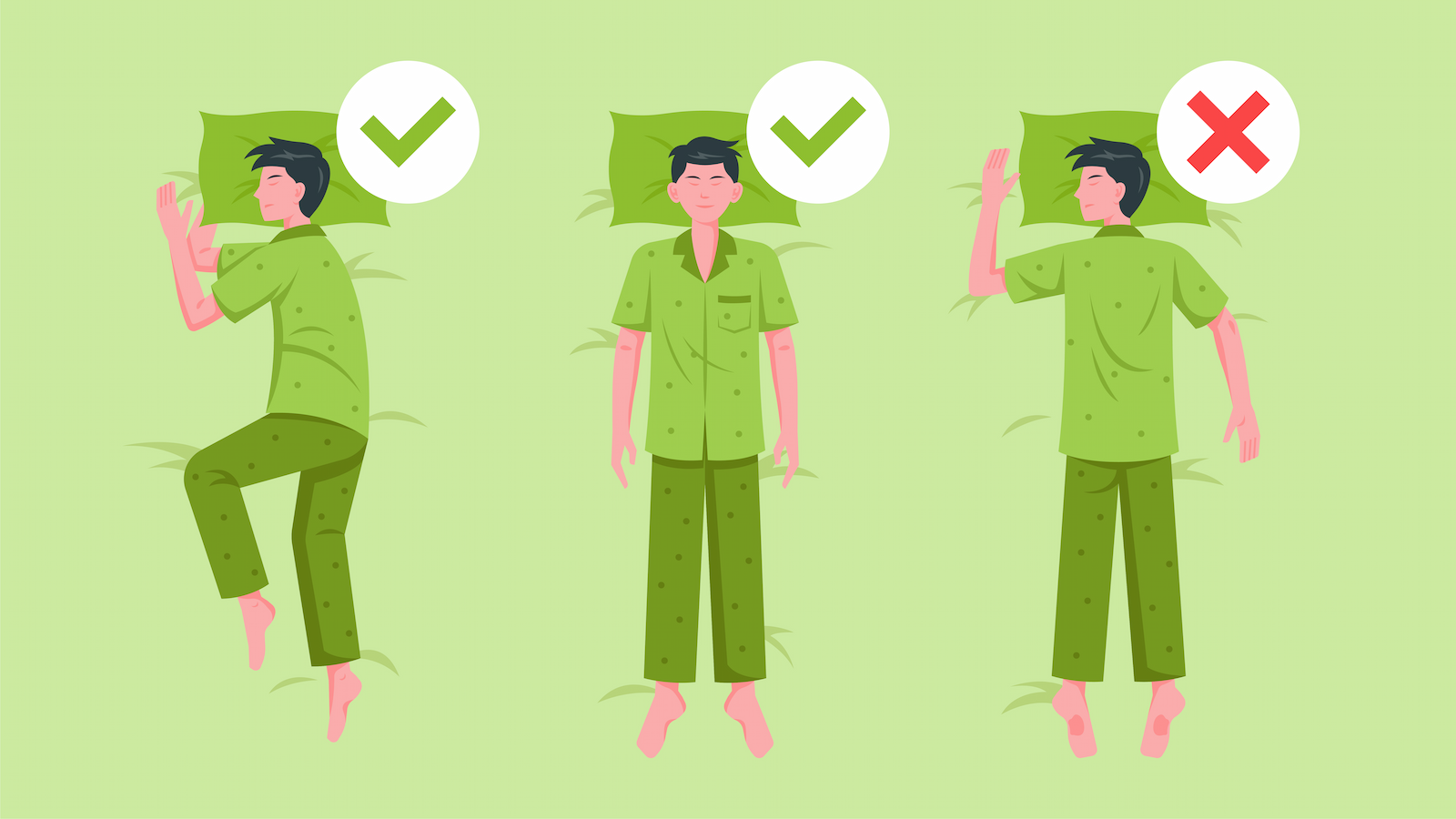
These positions are more likely to initiate apnea episodes. If you can, avoid sleeping on your stomach. This will ensure that your test records the most data possible. While moderate to severe cases might still show up on tests for stomach sleepers, mild apnea symptoms might not be as obvious.
Key Takeaways
- When conducted properly, at-home sleep apnea tests are just as reliable as lab-based tests for diagnosing moderate-to-severe obstructive sleep apnea cases.
- Since the tests might not detect mild sleep apnea cases, your doctor might still order additional testing if at-home test data is inconclusive.
- At-home tests focus on a limited set of data points, including breathing, airflow rates, blood oxygen levels, and heart rate.
- Home-based apnea tests typically use pulse oximeters, cannulas, and chest straps to gather data while you sleep in the comfort of your bed.
- At-home testing cannot diagnose other sleep or breathing disorders, such as circadian rhythm disorders, insomnia, hypersomnia, narcolepsy, breathing disorders, periodic limb movement disorders (PLMD), or restless leg syndrome (RLS)
- Once your doctor prescribes an at-home test, they should provide instructions on best administering the test.
- Avoid napping during the day or days you plan to gather data.
- Avoid caffeine and alcohol on the day or days you plan to gather data.
- Get comfortable and sleep as you usually would to encourage the most accurate results from your at-home sleep study.
If your at-home sleep study indicates that PAP therapy is right for you, CPAP Supply’s broad selection of industry-leading brands and comprehensive selection of accessories can help you get everything you need to start using your CPAP machine in one place. As Canada’s leading online CPAP supply store in customer satisfaction, we’re here to help you find exactly what you need! Browse our selection or contact us today!
References:
- Johns Hopkins Medicine: What To Know About an At-Home Sleep Test
- Sleep Foundation: At-Home Sleep Tests and Studies
- American Sleep Association: At-Home Sleep Apnea Test
- Sleep.org: Is a Home Sleep Study Right for You?
- University of Michigan Health: When is a Home Sleep Apnea Test Appropriate?
- Cleveland Clinic Health Essentials: Do You Need a Sleep Test? Ask Yourself These 8 Questions First
- American Association of Sleep Technologists (AAST): What is a Home Sleep Test?
- American Academy of Sleep Medicine (AASM): What is a Home Sleep Apnea Test?
- CleveMed: Home Sleep Testing – Everything You Need To Know
- Healthline: Which Type of Sleep Apnea Test Is Right for You?

