Sleep apnea often flies under the radar, especially in women, where it manifests in whispers rather than shouts.
It’s a silent intruder disrupting restful slumber, leaving a trail of fatigue and frustration in its wake.
This guide aims to highlight the often-overlooked sleep apnea symptoms in women, empowering you with the knowledge to spot the signs early.
Imagine this: a woman, let’s call her Sarah, juggles work, life, and myriad responsibilities.
She can’t shake off the cloak of exhaustion that clings to her, starting each day as tired as she ended the one before.

It’s only after years of attributing her tiredness to life’s hustle that she discovers the real culprit: sleep apnea.
Now, with the proper knowledge and tools, Sarah is on a path to reclaiming the restorative sleep she deserves.
Understanding sleep apnea is crucial. It’s not just about the snoring—though that’s a part of it—it’s about recognizing the subtle, nuanced symptoms that women experience.
This guide will walk you through these signs, explore the unique risks women face, and discuss the transformative impact of treatment.
Let’s demystify sleep apnea together, ensuring restful sleep is not just a dream for women like Sarah.
Understanding Sleep Apnea
Sleep apnea is more than just a disturbance in your sleep; it’s a serious sleep disorder where breathing repeatedly stops and starts throughout the night.
For many women, these interruptions are silent and go unnoticed, but the effects on the body and mind are anything but.
There are three main types of sleep apnea:
- Obstructive Sleep Apnea (OSA)
- Central Sleep Apnea (CSA)
- Mixed Sleep Apnea
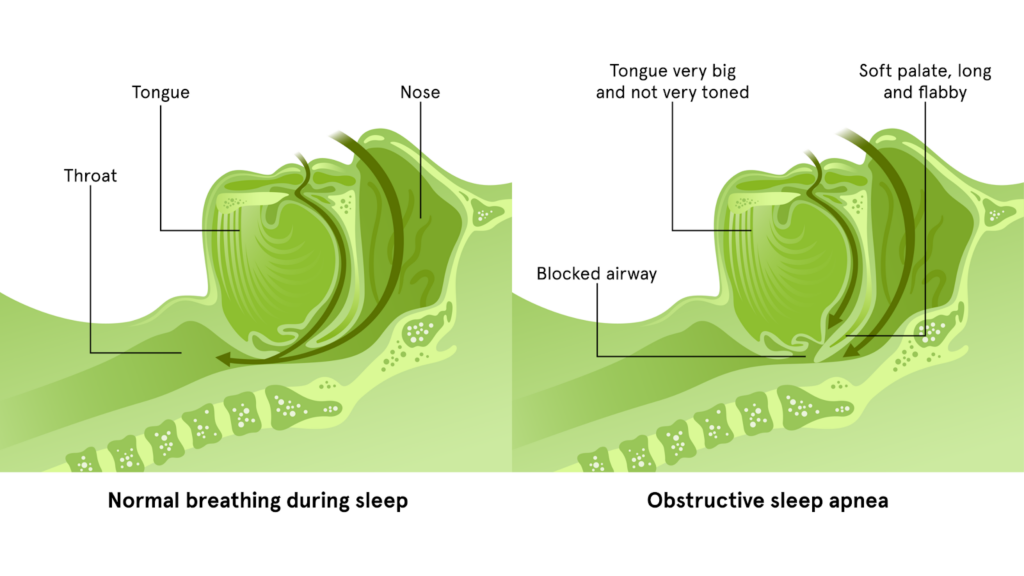
OSA, the most common form, occurs when the muscles in the throat relax excessively during sleep, leading to a blocked airway.
Women often experience sleep apnea differently than men.
While loud snoring is a hallmark sign in men, women may present with more subtle symptoms such as fatigue, insomnia, and mood disturbances.
These differences can make sleep apnea harder to diagnose in women, leading to a greater risk of it being overlooked or misattributed to stress or other health issues.
Understanding these nuances is the first step in recognizing and addressing sleep apnea in women.
With this knowledge, we can peel back the layers of this complex condition and reveal the complete picture of its impact on women’s health.
Symptoms of Sleep Apnea in Women
Recognizing the symptoms of sleep apnea in women is crucial for a timely diagnosis and effective treatment.
The symptoms can be subtle and, therefore, easily missed.
If you’re experiencing one or more of these symptoms, it may be time to consult a healthcare provider.
Nighttime Symptoms
Disrupted Sleep
Unlike the occasional restlessness everyone experiences, women with sleep apnea may find themselves waking up frequently throughout the night. This isn’t just tossing and turning; it’s a sudden jolt to consciousness that disrupts the sleep cycle and prevents deep, restorative sleep.

Snoring
While not all snorers have sleep apnea, persistent, loud snoring can be a sign, especially if silent pauses and gasping sounds accompany it. Snoring in women with sleep apnea may not be as loud as in men, making it an often-overlooked symptom.
Breathing Pauses
Bed partners are sometimes the first to notice episodes where the woman seems to stop breathing for short periods. These pauses, known as apneas, are a direct result of the airway being blocked during sleep.
Frequent Nighttime Urination
Known as nocturia, this can result from the body’s response to disrupted breathing. It’s not just about the bladder; it’s a complex interplay between sleep, breathing, and the body’s internal systems.
Daytime Symptoms
Unexplained Fatigue
Feeling tired after a whole night’s sleep can signal that the sleep was not as restful as it should be. Women with sleep apnea often experience this unexplained fatigue, which can significantly impact their daily activities.
Morning Headaches
These headaches can occur from the reduced oxygen levels in the blood caused by repeated interruptions in breathing. They are often a dull, throbbing sensation that can persist after waking.

Difficulty Concentrating
Sleep apnea can lead to poor sleep quality, which affects cognitive functions. Women may find it harder to focus and may suffer from memory issues due to disrupted sleep patterns.
Mood Changes
Irritability or mood swings may be more than just a bad day; they can be symptoms of sleep deprivation due to sleep apnea. The lack of quality sleep can affect emotional regulation and lead to feelings of depression or anxiety.
The Connection Between Restless Legs Syndrome and Sleep Apnea
Restless Legs Syndrome (RLS) and Sleep Apnea are two conditions that often intersect, particularly in women. Understanding this connection is vital, as it can impact the diagnosis and treatment of both disorders.
What is Restless Legs Syndrome?
Restless Legs Syndrome is a neurological disorder characterized by an uncontrollable urge to move the legs, typically due to uncomfortable sensations.
These feelings commonly occur in the evening or during inactivity, making it difficult to fall or stay asleep.
The Overlap with Sleep Apnea
Research in Movement Disorders indicates a significant overlap between RLS and sleep apnea.
The exact reasons for this connection are not fully understood, but the presence of one condition can often exacerbate the other.
For instance, the periodic leg movements of RLS can lead to fragmented sleep, which may worsen the symptoms of sleep apnea.
Why Women Should Pay Attention
For women, the link between RLS and sleep apnea is particularly important.
Hormonal changes, such as those occurring during pregnancy or menopause, can increase the risk of both conditions.

Women experiencing symptoms of RLS should also be screened for sleep apnea, as treating one can often relieve the other.
The Importance of a Holistic Approach
A holistic approach to treatment is essential.
Healthcare providers should consider the possibility of both conditions when a woman presents symptoms such as persistent leg discomfort at night and difficulty maintaining sleep.
Addressing both RLS and sleep apnea can lead to a significant improvement in sleep quality and overall health.
Fortunately, this is easier than it might sound, as research in Sleep Medicine indicates that PAP therapy—the gold standard treatment for sleep apnea—also shows signs of improving symptoms of RLS.
Understanding Risk Factors for Sleep Apnea in Women
While sleep apnea can affect anyone, certain factors can increase a woman’s risk of developing Obstructive Sleep Apnea.
Recognizing these can be the key to early detection and management.
Hormonal Changes: A Double-Edged Sword
Hormonal fluctuations during significant life events such as pregnancy and menopause can predispose women to OSA.
During pregnancy, increased progesterone levels can cause the upper airway to swell, leading to airflow obstruction during sleep.
Menopause brings a decrease in estrogen and progesterone, hormones that help maintain muscle tone in the throat, thus increasing the risk of airway collapse.
The Impact of Obesity
Obesity, particularly after menopause, is a significant risk factor for OSA.
Excess weight can lead to fat deposits around the neck and throat area, obstructing breathing at night.
Women must be aware of the changes in their body composition and metabolism, especially during and after the transition into menopause.
Lifestyle and Environmental Factors
Lifestyle choices such as smoking and alcohol consumption can exacerbate the likelihood of developing sleep apnea.
Environmental factors, including exposure to allergens or irritants, can also contribute to airway inflammation and subsequent sleep disturbances.
The Role of Genetics and Neck Circumference
Genetics play a role in the development of OSA, with certain inherited traits, such as the structure of the jaw and airway, making some women more susceptible.
Additionally, a neck circumference greater than 16 inches is often considered a risk factor for OSA.
The Consequences of Untreated Sleep Apnea in Women
The repercussions of leaving sleep apnea unmanaged extend far beyond mere sleep disturbances. For women, the consequences can be particularly severe, affecting various aspects of health.
Cardiovascular Complications
Untreated Obstructive Sleep Apnea can lead to a host of cardiovascular problems.
Women with OSA may experience:
- high blood pressure
- atrial fibrillation
- heart attacks
- strokes
The intermittent oxygen deprivation and the stress of repeated awakenings can affect the heart’s function over time.
Metabolic Syndrome and Type 2 Diabetes
Sleep apnea’s impact on metabolism can be profound.
The disrupted sleep patterns can lead to insulin resistance, a precursor to type 2 diabetes.
Women with OSA often struggle with glucose control, which can exacerbate metabolic syndrome and increase the risk of diabetes.
Pregnancy-Related Risks
For pregnant women, untreated sleep apnea poses risks not just to their health but also to the well-being of their unborn child.

Studies have linked OSA in pregnant women to complications such as gestational diabetes, preeclampsia, and low birth weight.
Mental Health and Cognitive Effects
The psychological toll of sleep apnea includes increased risks of depression, anxiety, and cognitive impairment.
The chronic tiredness that accompanies OSA can lead to mood swings, irritability, and difficulties in concentration and memory.
Addressing Sleep Apnea in Transgender Women
When discussing sleep apnea, it’s essential to consider the unique challenges faced by transgender women.
Hormonal therapy, anatomical factors, and the stress associated with gender dysphoria can all influence the prevalence and presentation of sleep apnea in this population.
Hormonal Therapy and Its Implications
Hormone Replacement Therapy (HRT), commonly used by transgender women, can have implications for sleep apnea, as highlighted in research published in the Journal of Clinical Sleep Medicine.

Estrogen and anti-androgens may affect fat distribution and muscle tone in the upper airway, potentially increasing the risk of OSA.
It’s essential for transgender women undergoing HRT to be monitored for signs of sleep apnea.
Anatomical Considerations
Transgender women may have anatomical characteristics, such as a larger neck circumference, which is a known risk factor for OSA.
This, combined with the potential effects of long-term testosterone exposure before transitioning, may contribute to a higher prevalence of sleep apnea.
The Stress Factor
The same Journal of Clinical Sleep Medicine research highlights how gender dysphoria and the stress associated with transitioning can lead to poor sleep quality and exacerbate sleep disorders, including sleep apnea.
Mental health support and stress management are crucial components of care for transgender women with sleep apnea.
A Tailored Approach to Treatment
Treatment for sleep apnea in transgender women may require a tailored approach that considers the impact of HRT, anatomical factors, and mental health.
Continuous Positive Airway Pressure (CPAP) therapy remains the cornerstone of treatment, but additional interventions may be necessary to address the unique needs of this population.
As always, consulting with your primary care provider or sleep specialist is the best way to ensure that any concerns about the specifics of your treatment plans are addressed promptly and thoroughly.
Differences Between Male and Female Experiences of OSA
The experience of Obstructive Sleep Apnea (OSA) can differ significantly between men and women, not only in symptoms but also in the journey to a correct diagnosis and effective treatment.
Gender Bias in Diagnostic Tools
Historically, sleep apnea research has focused predominantly on male subjects, leading to a diagnostic bias.
This has resulted in the development of assessment tools and diagnostic criteria more attuned to the typical male presentation of the disorder.
For instance, the emphasis on snoring as a primary symptom may overlook women who may present with fatigue or insomnia instead.
Personalized Approaches to Diagnosis and Treatment
Recognizing that women may exhibit different symptoms and have other anatomical and physiological considerations is crucial.
Women are more likely to have REM-related apnea. In this condition, breathing disturbances occur during rapid eye movement (REM) sleep, which is often associated with more severe symptoms of depression and anxiety.

A personalized approach to diagnosis should consider these differences.
For example, questionnaires and sleep studies may need to be adapted to capture the female experience of sleep apnea better.
Similarly, treatment plans should be tailored, taking into account factors such as hormonal fluctuations and potential pregnancy.
When to Consult a Doctor
Women should consult a doctor if they experience symptoms such as:
- Persistent daytime fatigue and unrefreshing sleep.
- Frequent awakenings or insomnia.
- Nighttime chest pain or palpitations.
- Morning headaches or dry mouth.
- Observations of breathing interruptions during sleep.
Early intervention is crucial in managing sleep apnea and mitigating its health impacts.
If you or someone you know is experiencing these symptoms, it’s important to seek medical advice quickly.
FAQs About Sleep Apnea Symptoms in Women
Can sleep apnea cause weight gain in women?
Yes, sleep apnea can lead to weight gain due to hormonal imbalances that affect appetite and metabolism, as well as reduced energy levels that can lead to decreased physical activity.
Are women less likely to snore if they have sleep apnea?
Women with sleep apnea may snore less loudly or less frequently than men, but this is not always the case. It’s important to note that not all women with OSA snore, and not all who snore have OSA.
How does menopause affect sleep apnea?
Menopause can increase the risk of developing sleep apnea due to hormonal changes that affect muscle tone in the throat and can lead to increased fat deposition around the neck area.
Can menopause therapy affect sleep apnea?
Hormone replacement therapy (HRT) during menopause can potentially affect sleep apnea.
Some studies suggest that HRT may help to maintain muscle tone in the airways and reduce the risk of sleep apnea, while others indicate it might increase the risk.
Women undergoing HRT should be monitored for sleep apnea symptoms and discuss any sleep-related concerns with their healthcare provider.
Can pregnancy increase the risk of developing sleep apnea?
Yes, pregnancy can increase the risk of sleep apnea due to hormonal changes, increased weight, and the physical effects of a growing uterus on the diaphragm.
Pregnant women experiencing symptoms like habitual snoring, frequent nighttime awakenings, or excessive daytime sleepiness should consult their healthcare provider.
Does sleep apnea affect women’s libido?
Sleep apnea can affect libido in women.
The chronic fatigue and sleep disruption caused by sleep apnea can lead to a decrease in sexual desire and arousal.
Furthermore, the associated hormonal imbalances may also play a role in reduced libido.
Are there specific sleep apnea symptoms that are unique to women?
While not entirely unique, specific symptoms such as fatigue, insomnia, morning headaches, and mood disturbances like depression or anxiety are more commonly reported by women with sleep apnea than men.
Women may also experience symptoms such as restless sleep and gasping for air that might not be as prevalent in men.
How does the treatment for sleep apnea differ between men and women?
The fundamental treatments for sleep apnea, such as CPAP therapy, do not differ between men and women.
However, the approach to treatment may be tailored to address specific needs, such as the use of different mask types or CPAP comfort settings, and considering factors like hormonal therapy in transgender women or those undergoing menopause.
Conclusion
Remember that recognizing and addressing sleep apnea is a crucial step toward better health and well-being, especially for women.
If you or someone you know is experiencing the signs and symptoms we’ve discussed, it’s not just about getting a good night’s sleep—it’s about taking control of your health and life.
Approach the subject with compassion and understanding. Encourage open conversations with healthcare professionals who can provide a proper diagnosis and a path forward.
There’s a world of support out there, and taking that first step towards consultation can lead to transformative outcomes.

For those ready to embark on this journey, CPAP Supply stands as a beacon of support.
Recognized as Canada’s leading online CPAP supply store in customer satisfaction, we understand the unique needs of women facing sleep apnea.
Our dedicated team is here to answer your questions and guide you through the selection of CPAP equipment, accessories, and supplies that cater specifically to women.
Don’t let sleep apnea dim the vibrant life you deserve. Together, we can ensure that every night leads to a brighter, more energetic tomorrow.
Take that step towards restful sleep and renewed vitality.
Contact CPAP Supply today, and let’s make good sleep a reality.
References
ScienceDirect: “Outcome of restless legs severity after continuous positive air pressure (CPAP) treatment in patients affected by the association of RLS and obstructive sleep apneas”
Movement Disorders: “Clinically significant but unsuspected restless legs syndrome in patients with sleep apnea”
ScienceDirect: “The urge to move and breathe – the impact of obstructive sleep apnea syndrome treatment in patients with previously diagnosed, clinically significant restless legs syndrome”
Sleep Better Georgia: “Restless Legs Syndrome & Sleep Apnea: The Connection & Treatment Options”
Respiratory: “Restless legs syndrome: impact on sleep-related breathing disorders”
European Respiratory Review: “Treating restless legs syndrome in the context of sleep-disordered breathing comorbidity”
PubMed: “Effects of restless legs syndrome (RLS) on sleep”
Mayo Clinic: “Restless legs syndrome – Symptoms and causes”
Journal of Clinical Sleep Medicine: “On Not Knowing What We Don’t Know to Knowing What We Don’t Know: Obstructive Sleep Apnea in the Transgender Community”
Chest Journal: “Restless Legs Syndrome: An Update on Prevalence, Pathophysiology, Diagnosis and Treatment.”
Sleep Medicine Reviews: “Gender differences in obstructive sleep apnea and treatment implications”
Drugwatch: “Gender differences in obstructive sleep apnea and treatment implications”
Sleep Foundation: “How Weight Affects Sleep Apnea”
Mayo Clinic News Network: “Mayo Clinic Q and A: Diagnosing sleep apnea”
Harvard Health Publishing: “Snoring and sleep apnea”
Everyday Health: “What Is Obstructive Sleep Apnea? Symptoms, Causes, Diagnosis, Treatment, and Prevention”
Verywell Health: “Sleep Apnea Treatment: Everything You Need to Know”
Consumer Notice: “Sleep Apnea”
National Heart, Lung, and Blood Institute: “What Is Sleep Apnea?”
Cleveland Clinic: “Sleep Apnea”
Sleep Foundation: “8 Health Benefits of Sleep”

