Central (CSA) and Obstructive Sleep Apnea (OSA) are significant sleep disorders that millions worldwide grapple with daily.
They both interfere with your breathing during sleep, but they do so in different ways.
It’s not just about snoring or feeling tired; it goes much deeper than that.
These conditions can profoundly affect your health and quality of life.

Understanding Central Sleep Apnea (CSA) and Obstructive Sleep Apnea (OSA) can help you recognize symptoms earlier.
As with many medical conditions, early detection of CSA and OSA may lead to more successful treatment plans, so it’s important to understand precisely what you’re dealing with.
So, let’s dive into this critical topic!
Understanding Central Sleep Apnea (CSA) and Obstructive Sleep Apnea (OSA)
Sleep apnea is a common condition. While exact numbers are unavailable, experts estimate that approximately 3 to 7 percent of men and 2-5 percent of women globally live with sleep apnea.
Given the current global population, this means potentially hundreds of millions of people are diagnosed with sleep apnea.
And this doesn’t include any undiagnosed cases going unnoticed and untreated.
However, not all forms of sleep apnea are created equal.
The disorder manifests primarily in two forms—central sleep apnea (CSA) and obstructive sleep apnea (OSA)—each with unique characteristics.
The Basics of CSA and OSA
We must first understand their core differences to explore these two types of prevalent sleep disorder.
- OSA is characterized by physical obstructions in the throat during slumber—often due to relaxed muscles—leading to airflow interruptions.
- CSA arises from an imbalance in brain signals controlling breathing patterns.
In terms of prevalence, Obstructive Sleep Apnea is by far the most common.
This makes understanding its root causes even more crucial for effective treatment strategies.
However, while less widespread than OSA, Central Sleep Apnea can pose equally serious health risks due to its neurological origins and sometimes baffling onset and symptoms.
Exploring the Causes of Central Sleep Apnea (CSA) and Obstructive Sleep Apnea (OSA)
The emergence of CSA and OSA can be attributed to numerous pre-existing medical issues, causes, and risk factors.
Here’s what you need to know.
Factors Leading to OSA
Physical obstructions in the throat often play a key role in the onset of obstructive sleep apnea.
One prime suspect? Excess weight can lead to additional pressure on the lungs and throat, swollen tissues and organs, and reduced muscle tone.
All of these make breathing during sleep more challenging.

In children, issues like enlarged tonsils or adenoids are common culprits behind this condition.
Even anatomical irregularities such as a narrow airway or deviated septum may amplify susceptibility.
Bear in mind that muscle tone naturally diminishes with age.
This relaxation might allow structures in your throat to collapse more readily when you’re asleep, causing interruptions in normal breathing patterns—an integral part of OSA.
However, not all causes are biological or physiological.
Sometimes, they’re due to habits and behaviours.
For example, consuming alcohol regularly—especially when in excess or before sleeping—can also cause diminished muscle tone and lead to developing apnea symptoms or amplifying existing conditions.
The Role of Brain Signals in CSA
Moving onto central sleep apnea, we find disrupted brain signals at its core instead of physical blockages or obstructions.
Essentially, the brain sporadically pauses sending the rhythmic signals to the muscles you use to breathe.

Since these actions are typically involuntary, the result is that your body stops attempting to inhale or exhale.
This form of apnea can be drug-induced and is often associated with opiates, linked directly with other serious medical conditions such as heart failure or stroke, or sometimes even associated with specific medical treatments—such as using a CPAP machine.
Understanding your exact triggers is essential for correct diagnosis and effective treatment plans.
Understanding Central (CSA) and Obstructive Sleep Apnea (OSA) Symptoms
Symptoms are the primary area where central and obstructive sleep apnea are similar.
Both forms can result in daytime sleepiness, morning headaches, trouble focusing, mood disorders, sexual dysfunction, weight gain, dry mouth, and more.
However, there is often one symptom that can act as a signal to let you know which type of sleep apnea you’re dealing with.
Loud Snoring: A Key Indicator of OSA
If you’ve been told that your snoring is disruptive or louder than usual, it may be more than an annoyance.
It could be a sign of OSA, as loud snoring often results from interruptions in normal breathing patterns caused by airway obstructions during sleep.
Should you start noticing any of the signs mentioned above, it’s crucial to take note and speak with your primary care provider or family physician.
Unraveling the Diagnosis Process for Central Sleep Apnea (CSA) and Obstructive Sleep Apnea (OSA)
Distinguishing CSA from OSA is a vital step in the diagnostic process.
Although these two types of sleep apneas share symptoms like excessive daytime fatigue or waking with a headache, their root causes set them apart.
Let’s look at the diagnostic process to see how they might differ between the two forms of sleep apnea and where they’re the same.
A Common Start: Symptom Quizzes and Discussion
Diagnosing either form will likely start with a quiz.
While this might be a form you fill out, often, it’s just a discussion with your family doctor.
The questions generally relate to typical signs associated with sleep disorders and will only take a few minutes to answer.
Your doctor will then compare your answers to other pieces of your health data, such as your weight, height, daily habits, overall health, and age, to determine if further exploration is required.
Paths Diverge: At-Home Tests vs Lab-Based Polysomnography
With a better idea of what you’re dealing with, your doctor might decide to investigate the potential for sleep apnea further.
If your doctor suspects obstructive sleep apnea and you live in a province that allows at-home sleep studies, there’s a strong chance your doctor will order one and explain the steps.
We have a complete guide on what to expect during an at-home sleep study.

The highlights typically include wearing a special device and a few accessories while sleeping and then turning it all back in for analysis when you’re done.
It’s surprisingly simple and convenient.
If your doctor suspects central sleep apnea—or your at-home test is inconclusive—your doctor might order a lab-based polysomnography test or sleep study.
These are less convenient as you’ll have to spend the evening at a sleep center or sleep laboratory, but the test is still non-invasive and painless—even if it is less convenient.
You can learn all about what to expect in our detailed guide to lab-based sleep studies.
But the short version is that you’ll arrive, and your lab technician will attach an array of sensors to you using sticky pads.
They’ll then ask you to lie down and try to sleep while collecting data throughout the night.
If your data is conclusive, they can make a diagnosis and prescribe therapy in a single visit.
Sometimes, a second study might be required to dial in treatment settings for maximum benefit.
Roads Converge Again: Sleep Study Follow-Ups
Regardless of the test administered, if the results come back conclusive, you’ll likely receive a call from your primary care provider.
Working with your sleep specialist, they’ll explain the results of your tests and begin to recommend treatment options—which we’ll talk about next!
Treatment Options for Managing Central Sleep Apnea (CSA) and Obstructive Sleep Apnea (OSA)
While CSA and OSA have similar symptoms, their treatments often differ significantly.
In fact, PAP therapy—the standard treatment for OSA—can exacerbate CSA symptoms.
In this section, we’ll look at the typical treatment options to give you an idea of what to expect after diagnosis with either of these disorders.
1. Positive Airway Pressure (PAP) Therapy
In essence, Positive Airway Pressure (PAP) machines maintain steady air pressure in your throat throughout your slumber, ensuring open airways.
Different machines are available that deliver air in different ways depending on your needs.
Two of the most common are Continuous Positive Airway Pressure (CPAP) and Automatic Positive Airway Pressure (APAP) machines.
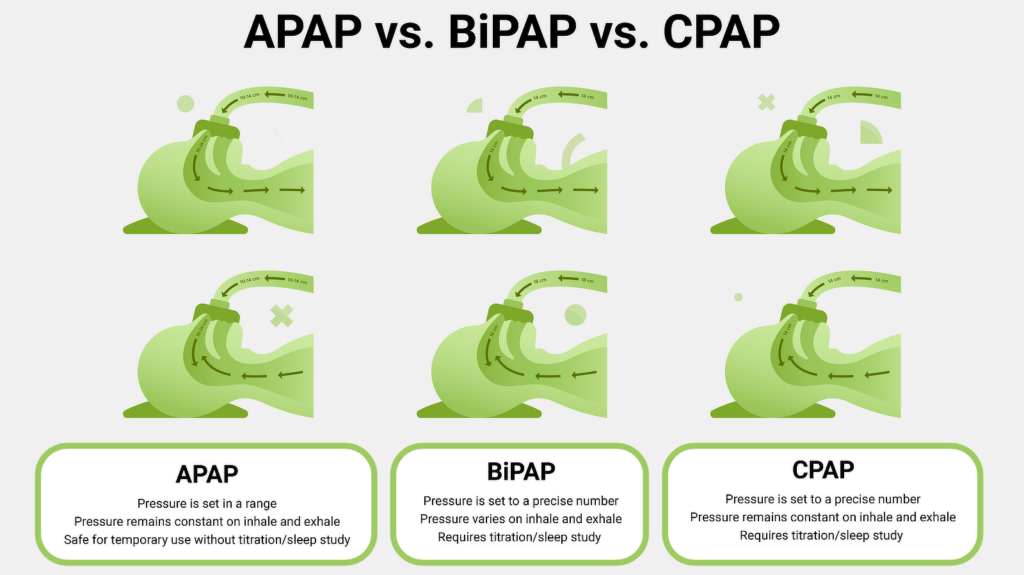
CPAP machines provide consistent pressure throughout treatment, while APAP machines can vary pressure throughout your therapy sessions based on apneas and hypopneas while you sleep.
But either can provide the level of adaptation needed to handle many CSA cases and could even result in the development of CSA in patients—a condition known as treatment-emergent central sleep apnea.
NOTE: You can learn more about the different types of PAP therapy available in our comparison guide.
2. Adaptive Servo-Ventilation (ASV) Therapy
Adaptive Servo-Ventilation (ASV) has similarities with APAP therapy in that it uses a stream of air to maintain breathing.
However, it’s much more personalized and complex, offering different pressures on inhale and exhale. It can even vary the pressure needed from breath to breath.
This means if it senses a pause in breathing, it can work to reestablish a regular breathing rhythm while minimizing the chances of triggering central sleep apnea episodes.
3. Alternative Treatment Methods
If PAP therapy doesn’t resonate with you or isn’t delivering desired results, don’t worry.
Alternative treatment options like oral appliance therapy might be just what you need.
Somewhat akin to wearing an orthodontic retainer or mouthguard during bedtime, this form of therapy aids in keeping your throat open by repositioning the jaw forward or preventing tongue obstruction—particularly beneficial for those grappling with OSA.
There are also potential surgeries to help address overly relaxed tissue that might be a good fit for your case.
Regardless of the alternative you wish to pursue, keeping your doctor or sleep specialist informed and part of your treatment journey can ensure you progress safely.
4. The Role Of Medication In Treating Sleep Apnea
While the fight against sleep apnea may sometimes involve medication, it is almost always an adjunct or secondary therapy, supporting PAP or ASV therapy alongside lifestyle adjustments and changes.

Here are a few potential uses for medication when addressing sleep apnea symptoms:
- Nasal decongestants, steroids, or antihistamines might be used short-term to deal with congestion-related discomfort. However, long-term use is discouraged.
- Medications such as modafinil sometimes help avoid excessive daytime sleepiness in the early stages. However, this isn’t directly treating sleep apnea and instead helping to support quality of life while addressing things in other ways.
- In severe OSA cases or when sleep apnea is comorbid with another respiratory condition such as COPD, doctors may prescribe supplemental oxygen alongside PAP therapy to assist in maintaining optimal oxygen levels.
In many cases, medications such as hypnotic sedatives, narcotic pain relievers, or muscle relaxers can actually worsen OSA symptoms and should be actively avoided.
Of course, the best source of information regarding the medications you should or shouldn’t take in relation to your sleep apnea is your primary care provider or sleep specialist. Always consult with them before changing your treatment plan.
FAQs About Central Sleep Apnea (CSA) and Obstructive Sleep Apnea (OSA)
Which is worse, CSA or OSA?
CSA and OSA are both serious conditions with potential health risks if left untreated. One is not inherently worse than the other—though CSA can be trickier to diagnose.
However, their severity can vary based on individual factors such as age, overall health status, and co-existing medical conditions.
Is central sleep apnea as dangerous as obstructive sleep apnea?
While both CSA and OSA carry health risks, OSA is generally considered more dangerous due to its association with high blood pressure, heart disease, stroke, and other cardiovascular conditions.
CSA has been less studied but can still negatively impact health.
You should not ignore either condition. If you suspect you or a loved one might have sleep apnea, consult a medical professional immediately.
Which is more common, OSA or CSA?
The most prevalent type of sleep apnea among adults is Obstructive Sleep Apnea (OSA), while Central Sleep Apnea (CSA) tends to be less common but equally significant.
Can you have both central and obstructive sleep apnea?
Yes, it’s possible to have a mixed presentation with components of both CSA and OSA.
This is known as complex sleep apnea and typically requires diagnosis via lab-based polysomnography and specialized PAP titration.
Can central sleep apnea go away on its own?
CSA may resolve when associated underlying conditions, like heart failure or opiate use, are effectively treated.
However, idiopathic CSA may be lifelong and require ongoing therapy.
Can you exercise with either central or obstructive sleep apnea?
Regular exercise is encouraged for OSA and CSA patients, as it helps manage weight, improve sleep, and lower cardiovascular disease risk.
Checking with your doctor first is advised to determine the best exercises to reach your goals without increasing health risks.
Can untreated sleep apnea lead to death?
Yes, untreated OSA raises the risk of fatal cardiovascular events.
CSA has also been linked to increased mortality, especially in heart failure patients.
Effective therapy can lower these risks.
Are sleep studies done at home reliable for central sleep apnea?
In-lab attended polysomnography is considered the gold standard for diagnosing CSA, as home sleep apnea tests may miss clinically significant respiratory events.
Conclusion
While they both originate in different areas of the body, obstructive and central sleep apnea can significantly impact your daily life—and long-term health—in similar ways.
Whether you are grappling with obstructive or central sleep apnea, the key is getting an accurate diagnosis and finding the best therapy for your situation.
Effective treatment can effectively manage OSA and CSA symptoms to improve health and quality of life.
But what works for one might not work for the other. So, consulting with a healthcare professional to help guide you through your treatment options is always the best option.
The team at CPAP Supply, Canada’s leading online CPAP store for customer satisfaction, is ready to help you find the right equipment, masks, and accessories tailored to your needs.
Contact us today to explore your options for regaining your energy, focus and well-being by taking control of your sleep apnea. CPAP Supply has the solutions and support to help you start sleeping soundly again.