Sleep apnea already impacts overall sleep quality, preventing you from waking rested and ready to take on your day.
But imagine not being able to sleep at all.
For many suffering from both sleep apnea and insomnia, this is an all-too-frequent occurrence.

This guide will explore the overlapping symptoms and shared risk factors of these two common sleep disorders and examine obstructive sleep apnea’s (OSA) impact on sleep quality.
We’ll also explore the role of continuous positive airway pressure (CPAP) therapy as an emerging treatment.
Join us as we navigate this intricate topic, shedding light on these conditions estimated to impact over a billion people worldwide yearly.
Understanding Sleep Apnea and Insomnia
Sleep apnea is a common yet often underdiagnosed condition, affecting a significant portion of the population.
It appears in two primary forms:
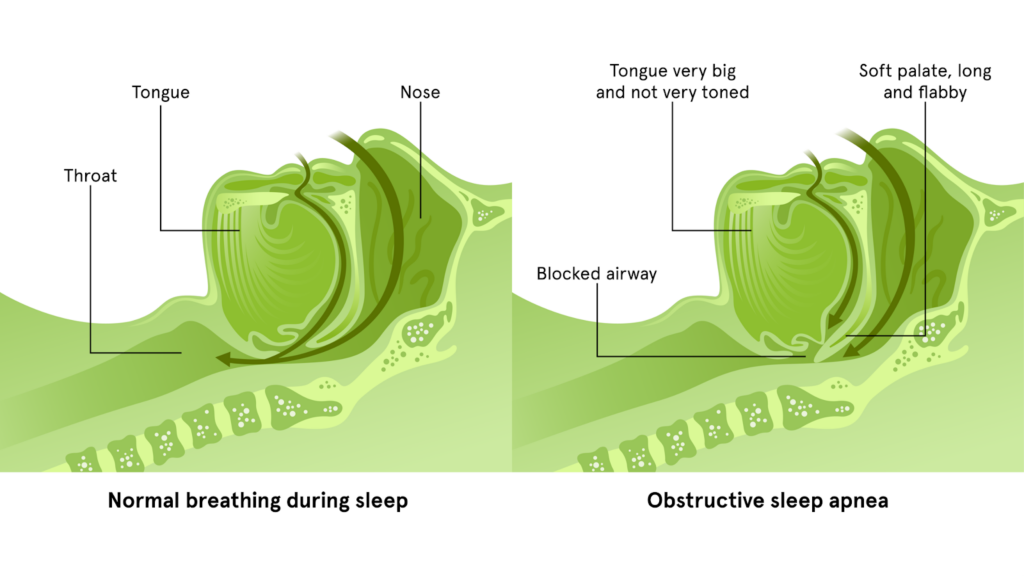
- Obstructive Sleep Apnea (OSA)
- Central Sleep Apnea (CSA)
OSA, the more prevalent of the two, occurs when the upper airway is obstructed during sleep.
On the other hand, CSA is characterized by the brain’s failure to send proper signals to the muscles controlling breathing.
For more information about how these two forms compare, be sure to check out our guide, “Understanding Central Sleep Apnea (CSA) vs Obstructive Sleep Apnea (OSA).”
Common symptoms include:
- Pronounced snoring
- Fragmented sleep
- Morning headaches
- Daytime fatigue
These symptoms can severely impact your quality of life, impacting nearly every corner of your world—including mood, energy levels, focus, productivity, and even sexual drive and performance.
Our guide, “Sleep Apnea Side Effects & Symptoms,” breaks down these symptoms in greater detail if you’re curious.
But for this guide, it’s essential to understand that many of these symptoms can intersect significantly with insomnia, further accentuating the effects of the disorders and making treatment more difficult.
Defining Insomnia in a Clinical Context
Insomnia is defined as difficulty falling or staying asleep despite adequate rest.
Insomnia is typically classified in one of two forms:
- Acute: often triggered by stress or life events
- Chronic: persisting for longer than three months
Experts have associated both acute and chronic insomnia with sleep apnea for various reasons.
Notably, both conditions share risk factors, such as advancing age and obesity.
Recognizing these shared risks is a simple way to bring your concerns to your primary care provider or sleep specialist. It is crucial in early intervention and effective management of sleep apnea and insomnia side effects.
The Interplay Between Sleep Apnea and Insomnia
The presence of sleep apnea can exacerbate the symptoms of insomnia, creating a cyclic pattern of poor sleep quality.
This correlation has been seen in study after study yet is often overlooked.
For new CPAP users, adjusting to the sensations of PAP therapy often leads to delayed or interrupted sleep and is a leading reason why people don’t stick with PAP therapy.
However, even if you’re well-adjusted to your PAP therapy equipment and routines, apnea episodes causing you to wake in the night and decreased sleep quality can also further contribute to insomnia symptoms.
Daytime Sleepiness and Its Role in Insomnia
Excessive daytime sleepiness, a hallmark of sleep apnea, is also a significant factor in the development and perpetuation of insomnia.
After a night of disrupted sleep due to apnea, you’ll often wake up sluggish and unrefreshed.
This leads to daytime drowsiness, which can impact not just energy levels but mood, habits, and sleep hygiene, further encouraging insomnia symptoms and furthering the cycle of poor sleep quality.
Impact of OSA on Sleep Onset and Maintenance
One of OSA’s less discussed but equally troubling aspects is its impact on sleep onset.
If you are experiencing frequent apnea episodes, you might struggle to transition from wakefulness to sleep due to their disrupted breathing patterns.
This difficulty in initiating sleep can be a direct contributor to insomnia, particularly onset insomnia.
How OSA Severity Impacts Insomnia Symptoms
There is also a noted connection between the severity of obstructive sleep apnea and the intensity of insomnia symptoms.
Studies suggest that the more severe the apnea episodes, the more significant the disruption to sleep, thereby exacerbating insomnia.
If you’re struggling to comply with your recommended PAP therapy regimen or still dialling in settings or fit with the help of your CPAP supply provider, sleep specialist, or primary care provider, you could find that you struggle with insomnia as well.
Bringing it up with your healthcare providers and support team can highlight options to minimize symptoms from both, helping you achieve compliance and further reduce symptoms.
Treatment Implications for Sleep Apnea and Insomnia
Continuous positive airway pressure (CPAP) therapy is a cornerstone in treating obstructive sleep apnea.
CPAP devices work by delivering a steady stream of air through a mask, keeping the airways open during sleep.

This reduces apnea episodes and improves overall sleep quality.
By minimizing breathing disruptions, CPAP not only aids in reducing daytime fatigue but also improves sleep onset and maintenance, which can be a game-changer for anyone also dealing with the effects of insomnia.
Addressing Both Conditions for Optimal Outcomes
If you’re experiencing symptoms of both sleep apnea and insomnia, it’s vital to adopt a holistic treatment approach.
CPAP therapy addresses the physical obstruction causing apnea, but managing insomnia often requires additional interventions.
This can include cognitive-behavioural therapy for insomnia (CBT-I), sleep hygiene education, and, in some cases, the prescription of sleep medication or supplements.
Fortunately, effective sleep apnea treatment with CPAP has been shown to improve insomnia symptoms, so these measures are often temporary.
Continuous support and follow-up are crucial to ensuring successful treatment outcomes, so if you run into any questions about how to best minimize the symptoms you’re experiencing—or if any part of your recommended treatment regimen doesn’t appear to be helping—be sure to consult with your primary care provider or sleep specialist for more information.
Shared Risk Factors and Lifestyle Modifications
A variety of lifestyle factors influence both sleep apnea and insomnia.
Combined with PAP therapy, addressing these shared risk factors can significantly improve your symptoms as well.
Weight management is crucial, as obesity is a known risk factor for both conditions. As such, emphasizing a healthy diet and ensuring you are physically active can go a long way in helping to resolve your symptoms.
Additionally, you should focus on developing good sleep hygiene practices.

This includes maintaining a regular sleep schedule, creating a comfortable sleep environment, and avoiding stimulants like caffeine and electronics before bedtime.
These lifestyle modifications, along with CPAP therapy, can significantly enhance your sleep quality, reversing this cycle and helping you build an improvement trend that results in better nights and better days ahead!
Frequently Asked Questions About Sleep Apnea, Insomnia, and CPAP Therapy
Can using a CPAP machine improve symptoms of insomnia?
By treating sleep apnea effectively, CPAP therapy can lead to better sleep quality and thus improve insomnia symptoms.
How can I tell if I have sleep apnea or insomnia?
Consulting a healthcare professional for a proper diagnosis is recommended, as they can assess symptoms and may suggest a sleep study.
Are there any specific populations that are more at risk for both sleep apnea and insomnia?
Apart from the general risk factors like obesity and age, certain populations, including menopausal women and individuals with certain medical conditions like hypertension and diabetes, are at a higher risk for both sleep apnea and insomnia.
Can psychological factors contribute to the development of insomnia in patients with sleep apnea?
Yes, psychological factors such as stress, anxiety, and depression can contribute to the development of insomnia.
For individuals with sleep apnea, the stress of chronic sleep disruption and fear of health consequences can further exacerbate insomnia.
How does sleep quality affect overall health in individuals with sleep apnea and insomnia?
Poor sleep quality can significantly affect overall health, leading to increased risks of cardiovascular disease, impaired cognitive function, mood disorders, and decreased immune function.
For those with both sleep apnea and insomnia, these risks are compounded.
Can sleep apnea be misdiagnosed as insomnia, and how can it be accurately distinguished?
Yes, sleep apnea can sometimes be misdiagnosed as insomnia due to overlapping symptoms like nighttime awakenings and difficulty maintaining sleep.
Accurate diagnosis often requires a sleep study to monitor breathing, oxygen levels, and sleep stages.
How does the treatment approach differ for someone with both sleep apnea and insomnia compared to someone with just one of these conditions?
Treatment for both conditions requires a more integrated approach.
While CPAP therapy is central for sleep apnea, additional treatments like cognitive-behavioural therapy, sleep hygiene education, and sometimes medication may be necessary to manage insomnia effectively.
Conclusion
In navigating the complexities of sleep apnea and insomnia, it’s clear that understanding and addressing these conditions is crucial for reclaiming a restful night’s sleep and improving overall well-being.
CPAP therapy can be a transformative solution, offering a beacon of hope for those trapped in the exhausting cycle of disrupted sleep and daytime fatigue.
However, the journey to optimal comfort and effectiveness with PAP therapy can be as individual as the people it serves.
That’s where CPAP Supply, Canada’s leader in customer satisfaction, steps in.
With a dedication to your health and a commitment to providing the highest quality service, CPAP Supply stands ready to assist you with any questions about your PAP therapy equipment or to offer guidance on optimizing comfort and ensuring solid sleep while using your CPAP machine.
Don’t let another restless night define your tomorrow. Reach out to CPAP Supply and take the first step towards a future of better sleep and brighter days.
References:
- Medical News Today: Is There a Link Between Insomnia and Sleep Apnea
- NIH: Insomnia and Obstructive Sleep Apnea
- Sound Sleep Health: Will Sleep Apnea Cause Insomnia
- CPAP.com: Sleep Apnea and Insomnia: Important Differences to Know
- Mayo Clinic: Sleep Apnea
- Healthline: What’s the Difference Between Insomnia and Sleep Apnea?
- Sleep Resolutions: Could My Insomnia and Sleep Apnea Be Related?
- AAFP: Obstructive Sleep Apnea and Chronic Insomnia Disorder: Updated Guidelines from the Va/DoD
- ResMed: Does Sleep Apnea Cause Insomnia?
- Mayo Clinic: Obstructive Sleep Apnea
- Healthline: The Affects of Sleep Apnea on the Body
- Goodpath: Insomnia and Sleep Apnea: What Are They?
- Sleep Dynamics: Is There a Link Between Insomnia and Sleep Apnea?
- Johns Hopkins Medicine: 4 Signs You Might Have Sleep Apnea
- Mayo Clinic: Insomnia
- Star Sleep and Wellness: Sleep Apnea and Insomnia: Is There a Connection?
- Sleep Centers: Sleep Apnea and Insomnia: How These Common Sleep Disorders Can Be a Deadly Combination
- The Strong Clinic: Can Sleep Apnea Cause Insomnia?
- Surviving Sleep Apnea: Does Sleep Apnea Cause Insomnia?

