Have you ever stirred from slumber like a bear just come out of hibernation?
You have no energy, your head is pounding, and the only evidence of sleep is the sound of your alarm blaring in your ears.
If this sounds familiar, you’re not alone.
Many folks with obstructive sleep apnea (OSA) feel exactly this way—tired even after what they thought was a whole night’s rest.
Understanding CPAP machine readings can be transformative for someone living with OSA.
These intricate yet essential numbers hold secrets to improving your sleep quality and overall health.
Today, we will break down complex terms, like the Apnea Hypopnea Index (AHI), discuss why pressure settings matter, and shed light on how these machines can sense airway conditions and leaks during treatment.
All this info aims to give you a better grip on your therapy.
Let’s dive in!
Understanding Obstructive Sleep Apnea, CPAP Therapy, and Data Monitoring
If you’re living with obstructive sleep apnea (OSA) or central sleep apnea (CSA), it can feel like you’re fighting a nightly battle.
This condition, considered severe when the number of disruptions per hour of sleep exceeds 30, affects your sleep quality and overall health.
You might wake up feeling tired even after what should have been a full night’s sleep.
The reason? Your airway repeatedly closes during sleep due to relaxed throat muscles or a deviated septum.
How can we prevent this from occurring?
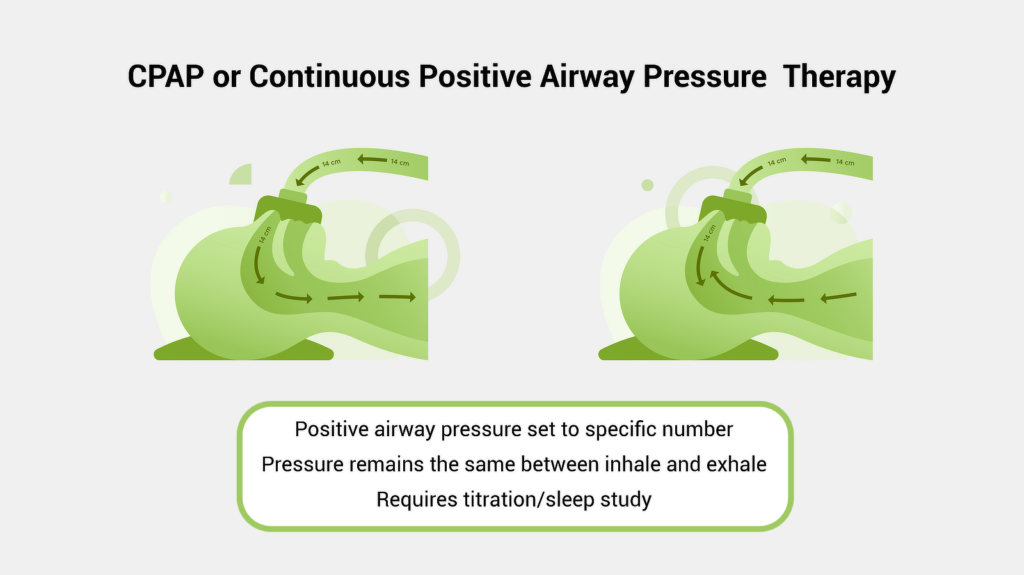
Continuous Positive Airway Pressure (CPAP) therapy comes to our rescue here.
A CPAP machine pumps pressurized air through a mask into your airway, keeping it open while you snooze away peacefully—assuming everything is working correctly, your CPAP mask fits well, and your settings are correct.
Personalization and PAP Therapy
As you might guess, it’s essential to tailor your machine, settings, and CPAP accessories to your specific needs to maximize the effectiveness of your treatment.
Too much pressure and it becomes uncomfortable.
But too little pressure, and it won’t prevent those pesky breathing interruptions effectively.
This is why having a sleep apnea test—also known as polysomnography—performed and a prescription issued outlining all of the settings needed for your machine.

During the titration phase of a sleep study, sleep specialists test different levels of air pressure settings during your sleep cycle until they find your Goldilocks pressure—the one that’s just right.
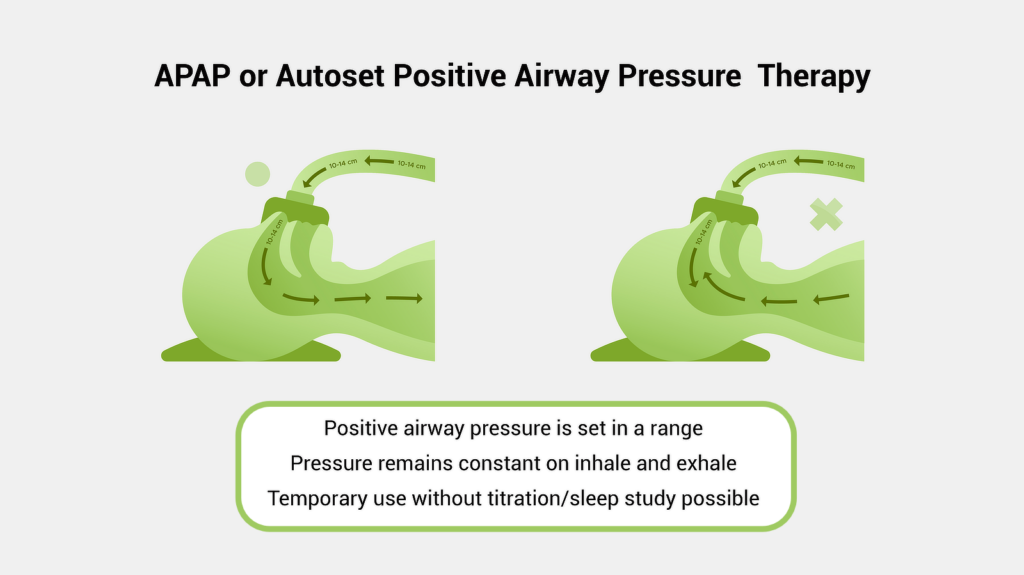
Depending on your machine, they might even be able to set it to a range of pressures to adjust your therapy based on your needs each night automatically.
You can learn more about different machine types in our guide: “PAP Therapies Compared: APAP vs. BiPAP vs. CPAP.”
The Importance of CPAP Machine Readings
For most PAP therapy patients, the change in symptoms once you’ve dialled in your fit and become comfortable wearing your mask each night is nearly immediate.
So immediate, many CPAP therapy users have trouble sleeping on vacation or travelling for work without their CPAP machine or if they forget to wear their mask one night after adjusting to treatment.
Understanding your CPAP machine readings is crucial for effective treatment.

These readings give valuable insight into how well you adhere to therapy and whether your current settings effectively treat your symptoms.
In this section, we’ll look at what type of data your machine likely collects before digging into how you might access and use it.
Usage Data from CPAP Machines
Your CPAP machine collects usage data throughout the night, recording vital information like air pressure settings, mask fitment, and leakage rates.
Today’s CPAP machines are smart devices. They don’t simply ensure a constant stream of pressurized air.
They also keep track of vital stats about your therapy sessions.
Older machines often store this data on SD cards or communicate directly with your doctor using mobile data.

However, many newer models collect and store the data on the device, making it easily accessible through mobile or computer apps.
This gathered data helps insurance companies and doctors assess if you’re sticking to the prescribed therapy regimen.
Typically, your doctors and insurance will want to see you using the device for at least 4 hours per night on 70% of nights in a given 30-day period—this might sound specific, but it’s pretty flexible.
In case you wonder why adherence matters so much, research shows consistent use improves overall health outcomes dramatically for CPAP users of all genders and ages.
Consistent use helps your doctors better dial in your settings and highlight other potential health concerns that might impact your quality of life.
Sticking with your therapy is essential.
Patient-Friendly Sleep Reports
But simply providing access to the data is only so helpful.
User-friendly data is far more useful.
Many modern CPAP machines offer just that with sleep reports—a simplified summary of your nightly therapy sessions.
A few taps can show key metrics like AHI (Apnea-Hypopnea Index), usage hours, and leak rates.
These are critical data points to understand how effective your treatment is in reducing or eliminating your apnea episodes and symptoms.
Decoding the Apnea Hypopnea Index (AHI)
The AHI score is a crucial piece of data in understanding sleep apnea.
It’s a number that represents how many times per hour you stop breathing or breathe shallowly during sleep.
Your sleep doctor will use your AHI reading to determine the severity of your condition and guide treatment options, such as CPAP therapy.
Understanding Your AHI Number
An AHI score under five is considered normal, while anything above that indicates some level of sleep apnea.
If your number falls between five and 15, it suggests mild obstructive sleep apnea.
However, an AHI reading from 15 to 30 signifies moderate OSA.
You’re likely dealing with severe sleep apnea if your index surpasses 30 events per hour—but don’t panic.
Effective treatments are available, like APAP machines, which adjust pressure according to need throughout the night’s sleep.
Also, lifestyle changes and additional medical support can often help reduce some of the causes of apnea, allowing you to work on lowering your AHI further.
Biological factors that can influence AHI include:
- Age
- Weight
- Gender
- Smoking
- Alcohol consumption
- Allergies
- Nasal congestion
- Jaw structure
- Tongue size
- Medical conditions such as heart disease, stroke, and diabetes
A Closer Look at What Influences Your Score
- Airway obstruction: CPAP machines use algorithms to detect both partial (hypopneas) and complete (apneas) respiratory obstructions based on subtle variations in airflow (source). In other words, it’s not just looking for large interruptions—it also keeps tabs on smaller disturbances, which can be equally disruptive to quality sleep.
- Sleep duration: Most adults need 7 to 8 hours of sleep per night. When you don’t get enough sleep, your body is more likely to experience stress. This can lead to an increase in the production of cortisol, a hormone that can narrow your airways and make OSA worse.
- Mouth Leaks: Mouth leaks occur when air escapes from your mouth while using a CPAP machine and breathing through your mouth with a nasal mask. Mouth leaks can reduce the air pressure delivered to your airway, which can make OSA worse or cause your machine to read apnea episodes inaccurately.
- CPAP mask Fitting: A well-fitting mask is essential for effective CPAP therapy. A mask that is too large or too small will not seal properly and will allow air to escape. This can reduce the amount of air pressure that is delivered to your airway and make OSA worse.
Evaluating Treatment Efficacy with Post-CPAP Therapy Readings
Post-therapy AHI scores are a key metric to gauge the effectiveness of your CPAP device.
A reduction in AHI and overall symptoms after CPAP therapy indicates effective treatment.
If your score remains high, seeing your doctor or sleep therapist to adjust your CPAP pressure settings and ensure you have the best mask for your sleep style and facial shape is important.
However, seeing the full benefits of using the CPAP therapy may take some time.
Some patients may notice an improvement in their symptoms immediately after starting treatment, while others may not notice a difference for several weeks or months.
Be patient, speak with your doctor or sleep therapist often to monitor your progress, and continue to attend any recommended follow-up appointments to improve your chances of compliance further and—ultimately—treatment success.
Detecting Air Leaks with CPAP Machines
But stats about your experience are only part of what your machine likely collects and reports.
Many models will also report back on how it detects that your equipment is performing.
Besides monitoring your breaths per minute (BPM), modern CPAP machines also keep track of any potential mask leak issues—both intentional leaks via exhalation ports designed into most masks for safety reasons and unintentional ones often caused by a poorly fitting mask or mouth leakage.
Total leak refers to the sum of intentional plus unintentional leaks—an excessively high total leak rate may indicate problems with mask fit or mouth leaking.
The occasional minor leak probably won’t impact your treatment too much and might not be worth worrying about in terms of time and cost to resolve.
But too much loss from an excessive leak could lead to inadequate treatment pressures while sleeping, meaning you’re not getting full benefits—if any—from your PAP therapy.
Many times, this measurement can also coincide with pressure readings.
CPAP machines are designed to deliver a specific amount of air pressure to keep your airway open.
If there is a leak in the system, the machine will have to work harder to maintain the desired pressure.
This can lead to an increase in pressure readings.
So, if you wake up feeling tired even after a full night’s sleep with your CPAP machine or notice your pressure readings creeping ever upward, it could be because of an air leak issue.
In such cases, consulting with a sleep doctor or CPAP supply provider can help pinpoint the problem and provide solutions to improve therapy effectiveness.
Accessing Your CPAP Machine Data
While exact steps will vary by model, most CPAP machines provide access to your sleep data in one of three ways:
- Using a memory card: Many CPAP machines have a slot for a memory card. You can insert a memory card into the slot and then download the data from the machine to your computer for analysis in various programs.
- Using Wi-Fi or Bluetooth: Newer CPAP machines can often connect to your phone or computer using Wi-Fi or Bluetooth. Some also connect to the Internet, storing your information in the cloud. This means that you can access your machine’s data easily without interacting with your CPAP machine physically.
Machines that support Wi-Fi, Bluetooth, or cloud storage often offer dashboards and reporting tools to access critical data at a glance.
Typically, this is transformed from the raw values reported by your machine into easy-to-read charts, graphs, or tables.
This makes it easier to understand what your readings mean without consulting your doctor about every detail.
However, the exact steps to use these apps will differ based on your CPAP machine manufacturer and the device you’re using the app on.
As such, step-by-step details are outside the scope of this guide.
However, if you need help using the mobile app that interacts with your CPAP machine, consulting your manufacturer’s website or speaking with your CPAP supply provider are excellent starting points.
FAQs About CPAP Machine Readings
What is a good reading on your CPAP machine?
This will vary by person. However, a lower AHI score than before you started therapy shows that your CPAP settings and treatment are effective. In most cases, doctors recommend reaching an AHI of five or lower.
What is a good number of events per hour with CPAP?
Fewer than five sleep disruptions (apneas or hypopneas) an hour signals solid control over sleep apnea with your CPAP.
What is considered a high CPAP pressure?
Above 15 cmH2O indicates high pressure in most cases. But it’s best to follow what your doctor recommends for you.
What is the proper flow rate for a CPAP machine?
The ideal flow rate differs by person and condition severity. However, most folks need between 6-14 cmH2O for optimal results.
Why is it important to review my CPAP machine data?
It is important to review your CPAP machine data to ensure that your CPAP therapy is working and that you are getting the most out of it.
You should also talk to your doctor or sleep therapist if you have any questions about your data or are concerned about any readings.
What is the difference between AHI and leak rate?
The AHI measures the number of apneas and hypopneas per hour of sleep. The leak rate measures how much air is escaping from the face mask while the CPAP machine is in use.
What should I do if my AHI score is not improving with CPAP therapy?
Schedule a follow-up appointment with your doctor if your AHI score remains high after starting CPAP therapy.
They may need to adjust your pressure settings or equipment to treat your apnea better.
Adherence, mask fit, and lifestyle factors can also impact results.
Why does my CPAP pressure feel too high or low?
Consult your doctor if the pressure feels uncomfortable. Your settings may need adjustment. Lifestyle changes can also impact ideal pressure over time.
Conclusion
The path to restful slumber may seem elusive when living with sleep apnea, but help is out there.
When properly set up and followed diligently, modern CPAP therapy can be life-changing—restoring that sweet sensation of waking up refreshed and energized.
While decoding CPAP data may feel overwhelming initially, access to your personal sleep metrics allows you and your care team to tailor therapy to your needs better.
With some guidance on key terms, these numbers transform into powerful insights for improving sleep quality and overall well-being.
If the complex world of CPAP readings still has you puzzled, rest assured that resources exist to help make sense of it all.
As Canada’s leading online CPAP equipment provider in customer satisfaction, CPAP Supply offers unmatched customer support and expertise.
Our caring staff is always happy to answer your CPAP questions, ensure you have the optimal equipment, and help you gain the full benefits from therapy.
Sleep apnea will not get the last laugh.
Consistent CPAP use, an understanding of your data, and personalized support arm you with the tools needed to reclaim those lost nights.
The opportunity for deep, restorative sleep is closer than you think.
Reach out today to start your journey toward sweet dreams once again.
