For individuals experiencing allergies and sleep apnea, understanding the connection between these two conditions is crucial in managing their symptoms effectively.
In this blog post, we will explore the intricate interplay between allergic rhinitis (also known as hay fever when seasonal) and obstructive sleep apnea (OSA), examining how they can affect each other’s symptoms.
We will discuss the impact of nasal inflammation on airway obstruction and examine how certain allergy medications may exacerbate OSA symptoms.
We’ll also explore alternative safe treatments for those with allergies looking to prevent sleep apnea complications.
Furthermore, you’ll learn about CPAP therapy safety for people with allergies, including mask types specifically designed to accommodate allergy sufferers.
We will highlight treatments that address both conditions while emphasizing the importance of effective allergen control in improving CPAP therapy results.
Lastly, we’ll provide practical lifestyle changes to help manage allergies and sleep apnea complications—from reducing indoor allergens to maintaining separate sleeping quarters for pets if they contribute to allergic reactions.
By understanding these connections and implementing appropriate strategies, you can achieve a better quality of life despite dealing with both conditions.
Let’s dive in!
NOTE: We’re not licensed medical professionals; this should not be considered medical advice. Individual responses to any medication or medical treatment will vary from individual to individual based on a range of factors we can’t possibly account for in a single article. This content is meant to inform you of possible options and provide a starting point for understanding the topic. If you have questions, a qualified medical professional is always your safest and most reliable source of information.
The Relationship Between Allergies and Sleep Apnea
Research has shown a positive association between these sleep apnea and seasonal allergies, with allergy patients often experiencing sleep-disordered breathing due to nasal mucosa edema (also known as nasal inflammation) and congestion.

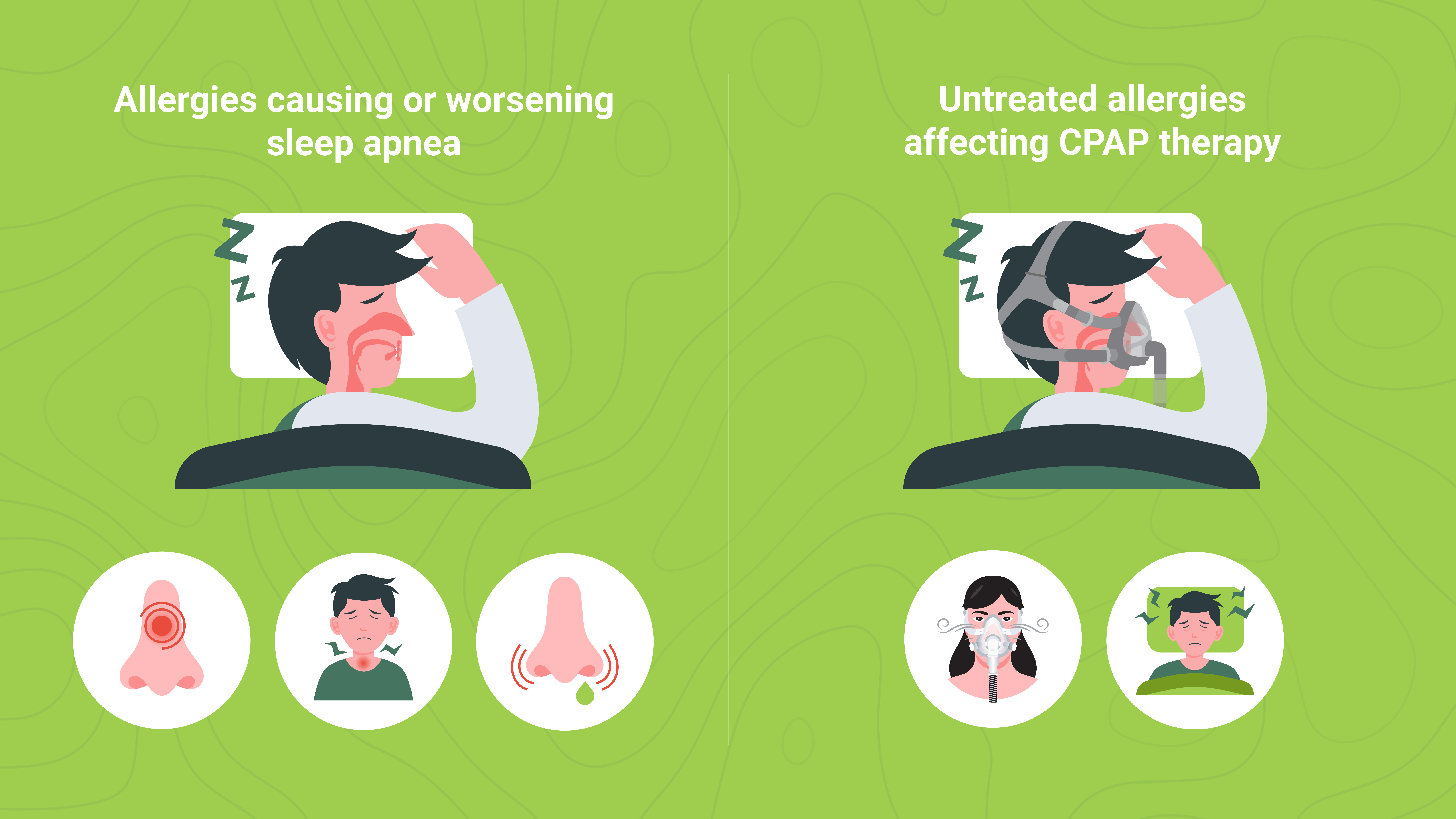
How Allergies Can Cause or Worsen Sleep Apnea
Hay fever is a well-known issue with sleep apnea patients because of its three core symptoms:
- Nasal Congestion: The swelling of the lining inside your nose caused by allergic reactions makes it difficult for air to pass through freely.
- Inflammation: In response to allergens like pollen or dust mites, your immune system releases chemicals that cause inflammation in affected areas such as the throat and sinuses.
- Mucus Production: Allergy sufferers often produce more mucus than usual during an allergic reaction, which can further obstruct airflow while sleeping.
Since obstructive sleep apnea (OSA) occurs when the airway is impeded or blocked while sleeping, hay fever can easily contribute to this blockage and either cause or worsen existing sleep apnea.
The Impact of Untreated Allergies on CPAP Therapy
If left untreated, allergies don’t just increase the risk of developing obstructive sleep apnea but can also interfere with the continuous positive airway pressure (CPAP) therapy methods used to treat apnea symptoms.
CPAP machines deliver a steady stream of air through a mask to keep your airways open during sleep.
However, untreated allergies can make it difficult for the machine to provide effective treatment due to the following:
- Poor Mask Seal: Allergy symptoms like watery eyes and runny nose can cause difficulty achieving a good seal with your CPAP mask or cause you to remove your mask frequently, leading to reduced therapy effectiveness..
- Discomfort and Poor Sleep Quality: Allergy symptoms such as sneezing, itching, or coughing can disrupt a good night’s sleep even when using a CPAP machine. A lack of restorative sleep further contributes to daytime sleepiness and other adverse effects of untreated obstructive sleep apnea.
Treating allergies is essential for improving overall health and can prevent sleep apnea symptoms from increasing.
Managing Allergies While Using CPAP Therapy for Sleep Apnea
By addressing allergy symptoms proactively through medications or lifestyle changes, you’ll increase the likelihood of experiencing better quality rest each night, minimize potential complications related to untreated allergies and sleep apnea, and ensure that your treatment is as effective as possible in relieving the symptoms of sleep apnea.

Here are some five practical tips to help you manage your allergy symptoms during CPAP therapy:
- Keep your windows closed during the day: Allergy sufferers often experience worsened symptoms when pollen counts are high. Close windows during the day to minimize exposure to allergens, improving sleep quality at night. This will help reduce indoor allergen levels and encourage a good night’s sleep. If you cannot keep your windows closed, installing high-quality air purifiers with hypoallergenic or HEPA filters can help minimize environmental allergens.
- Shower before bed each night: Bathing before bedtime can be highly effective for those with allergic rhinitis or hay fever. It eliminates allergens such as pollen and pet dander from the body and hair and limits their transfer to your bed linens and sleeping environment. This leads to easier breathing during sleep and fewer apnea complications. A warm shower may also aid in opening up nasal passages, further boosting the effect. Not to mention the relaxing effects. Allergies and sleep apnea aside, it could simply help you fall asleep faster.
- Sleep separately from pets if possible: Pets, especially cats and dogs, can carry allergens like pet dander and pollen. These allergens can irritate your airways, leading to increased inflammation and congestion. This can exacerbate sleep apnea symptoms, as a narrowed airway increases the likelihood of breathing obstructions during sleep. They can sometimes make it harder to stay asleep should they want to play during the night, are prone to loud snoring, hear a noise outside your bedroom window, or have vivid dreams that lead to noises and motion.
- Regularly groom and bathe pets: Regularly bathing your pets is essential to reducing allergens in your home, improving your overall health, and potentially alleviating sleep apnea symptoms. Not only does this cut down on loose hair and dander, which animals naturally produce, but if your pet frequently goes outside, regular bathing can also drastically reduce the transfer of pollen and other seasonal allergens from your yard into your home.
- Utilize hypoallergenic mattress and pillow covers: By creating a barrier against common allergens like dust mites, pet dander, and pollen, hypoallergenic covers contribute to a cleaner, more comfortable sleep environment, further enhancing sleep quality and overall health.
These strategies can help you better manage your allergy symptoms while using CPAP therapy for sleep apnea.
This will help improve your treatment’s effectiveness and contribute to a good night’s sleep and overall well-being.
Safety Concerns When Using a CPAP Machine With Allergies
When you have allergies and sleep apnea, knowing the safety aspects of using a CPAP machine is important.
Understanding any potential risks and taking steps to mitigate them will improve treatment outcomes while helping you alleviate and minimize your allergy symptoms.
Allergy sufferers may experience increased nasal congestion or irritation when using a CPAP machine if allergens are introduced into their airways through the mask.
This can lead to obstructive sleep apnea episodes, reduce therapy effectiveness, and reduce your comfort.
Each of these things, in turn, can then lead to reduced compliance as you skip wearing your mask, looking for relief.
The result is greatly diminished benefits and a lower overall quality of life.
While the tips outlined in the previous section can help immensely reduce the allergens in your sleeping environment, you must also consider ways to minimize the allergens collected in your CPAP machine.
Since the machine provides a pressurized stream of air directly into your nose and mouth, dirty masks or tubing can harbour allergens like mould spores or bacteria which could trigger an allergic reaction while wearing the device at night.
While maintaining clean equipment is essential for all CPAP machine users, it’s particularly important for improving the comfort and safety of your CPAP machine if you experience allergies and sleep apnea.

Here are some tips on keeping your CPAP supplies clean:
- Cleanse your face before putting on the mask each night: Washing your face with a gentle cleanser removes excess oils, dirt, and makeup, which can otherwise accumulate on the mask cushion and reduce its effectiveness. Clean skin also helps the mask seal properly, ensuring optimal therapy.
- Clean your CPAP mask, tubing, and humidifier chamber regularly according to the manufacturer’s instructions: Cleaning these components prevents the buildup of bacteria, mold, and allergens. The mask cushion should be cleaned daily, while the tubing and humidifier chamber should be cleaned weekly. Ensure all parts are thoroughly rinsed and dried before reassembling.
- Replace filters as the manufacturer recommends: CPAP devices have filters that help ensure clean air is delivered during therapy. Regularly replacing these filters, usually every 1-3 months or as instructed, prevents allergens and particles from entering your airways and causing irritation.
- Avoid harsh chemicals or scented cleaning products: These substances can leave residues on your CPAP equipment that may irritate when inhaled. Stick to gentle, unscented soap or cleaners specifically designed for CPAP equipment.
- Inspect your equipment regularly: Check for signs of wear and tear, such as cracks or tears in the mask or tubing. Damaged equipment can compromise the effectiveness of your therapy and should be replaced.
- Store your CPAP equipment properly: Keep your device and accessories in a clean, dry, and dust-free location when not in use to minimize exposure to allergens and contaminants.
Not sure how to clean your CPAP equipment?
Our guide to CPAP cleaning and maintenance fundamentals has you covered!
These precautions will help you safely use a CPAP machine while managing allergies and sleep apnea.
Remember to consult your healthcare provider if you have concerns about potential complications or need assistance finding allergy-friendly equipment options for sleep apnea treatment.
Best Types of CPAP Masks for People With Allergies
If you experience allergies and sleep apnea, your CPAP mask choice can greatly influence comfort levels during treatment.
In this section, we will explore different types of masks designed specifically for people with sensitivities so they can find an appropriate fit.
Full Face Masks
These cover your mouth and nose, providing a secure seal that helps prevent air leaks.
They are ideal for individuals who experience nasal congestion due to allergies or have difficulty breathing through their nose at night since you can easily switch between mouth breathing and nose breathing as congestion levels change.
These masks typically provide a secure seal but may feel more restrictive than other mask designs.
Their larger skin contact areas could also cause increased skin irritation, so optimizing your mask fit is essential.

Some popular full-face masks include:
- ResMed AirFit F30i
- Respironics DreamWear Full-Face Cushion Mask
- ResMed AirFit F20 Full Face CPAP Mask
- ResMed Mirage Quattro Full Face CPAP Mask
- Fisher & Paykel Evora Full Face CPAP Mask
You can learn more about these leading CPAP mask options in our guide, Exploring the Top Full Face CPAP Masks.
Nasal Pillow Masks
These lightweight masks feature small cushions that rest under your nostrils, allowing direct airflow into your nasal passages.
They suit allergy sufferers who prefer minimal facial contact or have sensitive skin prone to irritation from larger masks.
They’re also often much lighter than full-face masks due to the cushion’s reduced surface area and mass.

However, a nasal mask might be less effective if you have severe nasal congestion, a deviated septum, or primarily breathe through your mouth during sleep.
Some popular nasal pillow masks include:
- ResMed AirFit P10 Nasal Pillow CPAP Mask
- Fisher & Paykel Brevida Nasal Pillow CPAP Mask
- Respironics Dreamwear Silicone Nasal Pillow CPAP Mask
- ResMed AirFit P30i Nasal Pillow CPAP Mask
- ResMed Swift FX Nasal Pillow CPAP Mask
Want to know more about these top-selling CPAP mask models? Consult our guide, CPAP Masks: Top Nasal Pillow CPAP Masks Explored.
A Note for CPAP Users with Sensitive Skin
The materials used in CPAP masks and headgear can significantly impact the comfort and overall therapy experience for sleep apnea patients with sensitive skin.
In addition to mask design, consider the following to reduce the risk of skin irritation or allergic reactions when choosing a mask and headgear:
- Mask materials: Look for equipment made from hypoallergenic materials, as they are less likely to cause skin irritation or allergic reactions. Examples include silicone, gel, memory foam, and soft cloth materials. Patients with sensitive skin might find gel or memory foam cushions are more comfortable and less irritating while providing a more conforming seal.
- Headgear materials: Headgear made from soft, breathable fabric can be a more comfortable choice for sensitive skin, as it reduces the likelihood of chafing or pressure sores.
- Adjustable straps: Look for headgear with easily adjustable straps to optimize your mask fit. A proper fit reduces pressure on sensitive areas and prevents overtightening, which can increase discomfort and skin irritation.
Selecting suitable CPAP mask and headgear materials, along with adjustability features, is crucial for sleep apnea patients with sensitive skin, ensuring a comfortable and effective therapy experience while minimizing skin irritation and allergic reactions.
The Impact of Allergy Medications on Sleep Apnea Symptoms
While you’ve probably considered how allergy symptoms might impact your sleep apnea and PAP therapy experience, you might not have considered how your allergy medications interact with your therapy.
But there are effects you’ll want to understand as this knowledge can also help you to remain vigilant for anything you might want to bring up with your sleep specialist or primary care provider.
Antihistamines and Sleep Apnea
Antihistamines, such as cetirizine (Zyrtec) or loratadine (Claritin), are commonly used to treat seasonal allergies.
They block histamine receptors in the body that cause the most prevalent allergy symptoms, including runny nose, watery eyes, and nasal congestion.

Benefits include:
- Reduced allergy symptoms: Antihistamines can alleviate sneezing, itching, and nasal congestion. By reducing nasal congestion, antihistamines may improve breathing and prevent sleep apnea symptoms from compounding with allergy symptoms.
- Easier CPAP use: With reduced nasal congestion and allergy symptoms, sleep apnea patients may find it easier to use and tolerate their CPAP devices, leading to more effective therapy.
- Improved sleep quality: Allergy symptoms can cause sleep problems. By alleviating these symptoms, antihistamines may improve sleep quality for allergies and sleep apnea.
But they’re not perfect.
There are some important side effects and potential interactions to keep in mind, including:
- Sedation: Some antihistamines, particularly first-generation ones, can cause drowsiness or sedation. This side effect can exacerbate sleep apnea symptoms by relaxing the throat muscles and increasing the likelihood of airway obstruction. It can also create further issues if you already struggle with daytime drowsiness—a common sleep apnea symptom.
- Dry mouth and throat: Antihistamines can cause dry mouth and throat, worsening sleep apnea symptoms by contributing to airway irritation and increasing the risk of obstruction.
Nasal Decongestants and Sleep Apnea
Nasal decongestants, such as pseudoephedrine (Sudafed) or oxymetazoline (Afrin), aim at relieving nasal congestion by narrowing blood vessels in the nasal passages.
However, they should be used cautiously if you have obstructive sleep apnea because they can increase heart rate and blood pressure, potentially worsening sleep apnea symptoms.

Benefits include:
- Relief from nasal blockage: Less resistance due to congestion when breathing may potentially lessen sleep apnea symptoms related to nasal obstructions.
- Increased CPAP comfort: By alleviating nasal congestion, individuals with sleep apnea might find their CPAP devices more comfortable and easier to tolerate, resulting in more effective treatment.
- Enhanced sleep experience: Alleviating nasal congestion using decongestants can improve the sleep experience for sleep apnea patients by reducing sleep disruptions caused by difficulty breathing through the nose.
However, much like with antihistamines, using nasal decongestants when you have sleep apnea can have some downsides as well, including:
- Increased blood pressure: Decongestants can raise blood pressure, which may concern sleep apnea patients with an increased risk of hypertension and cardiovascular issues.
- Insomnia: Some decongestants, particularly those containing stimulants like pseudoephedrine, can cause insomnia, restlessness, and other sleep disorders, negatively impacting sleep quality.
- Short-term relief: Decongestants generally provide temporary relief, and prolonged use can lead to rebound congestion, making symptoms worse when the medication is discontinued.
When to Consult Your Doctor About Medication Adjustments
If you’re worried about the impact of your allergy medications on sleep apnea symptoms or CPAP therapy, it’s essential to consult a healthcare provider for adjustments and alternative treatments.
They can review your current medications and make any necessary adjustments based on the severity of both conditions.
Additionally, they may recommend alternative treatments like allergy shots, air purifiers, or natural remedies that won’t interfere with existing medications and allow you to manage your sleep apnea more effectively.
In some cases, a referral to an allergist or immunologist might be beneficial for more specialized testing and treatment options tailored specifically to address both allergies and sleep apnea.
Allergy Shots as a Long-Term Solution for Sleep Apnea Patients
Allergen immunotherapy, also known as allergy shots, is a long-term treatment for allergic reactions that reduces sensitivity to specific allergens.
It involves administering gradually increasing doses of the allergen(s) to help the immune system build tolerance, ultimately decreasing allergic symptoms.
The gradual treatment process requires regular injections over several months to years.
Typically the exact allergens administered are determined using a series of tests that determine the type of reactions you experience and their severity.
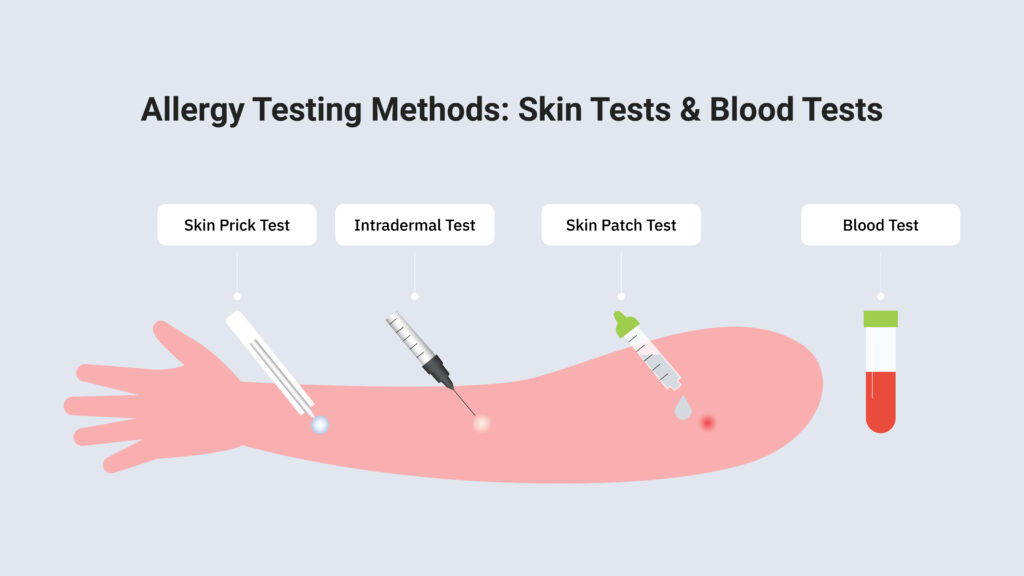
Allergy testing typically involves two primary methods: skin tests and blood tests.
Skin tests are the most common method for allergy testing.
They involve introducing small amounts of potential allergens to the skin to observe if a reaction occurs using one of three methods:
- Skin prick test: Small drops of allergen extracts are placed on the skin, usually on the forearm or back, and then the skin is gently pricked or scratched to allow the allergen to penetrate the skin’s surface.
- Intradermal test: An allergen extract is injected beneath the skin’s surface. This method is typically used if the skin prick test is inconclusive.
- Skin patch test: Allergen extracts are applied to patches, which are then placed on the skin and left for a period (usually 48 hours) to check for a reaction.
Blood tests, such as the ImmunoCAP or ELISA test, measure the levels of allergen-specific antibodies in the blood.
Blood tests are generally used when skin tests are unsuitable, such as in cases of severe skin conditions, a history of severe allergic reactions, or when using medications that interfere with skin testing.
In the context of sleep apnea, allergen immunotherapy can benefit you if allergies, particularly nasal congestion, exacerbate sleep apnea symptoms.
Immunotherapy may improve breathing during sleep and alleviate sleep apnea symptoms by reducing allergic reactions and nasal congestion severity.
It is important to note that allergen immunotherapy is not a direct treatment for sleep apnea but an adjunct therapy that addresses allergy-related factors that can worsen sleep apnea.
As with most medical treatments, the first step in determining if allergen immunotherapy is appropriate for your situation is to consult a medical professional.
Other Popular Recommendations for Allergies and Sleep Apnea
Managing both allergies and sleep apnea can be challenging.
Still, if over-the-counter antihistamines or nasal decongestants aren’t working—or you want additional options—you might find that your sleep specialist or primary care provider can provide feedback on different options that might bring relief.
Of course, there are also homeopathic, natural, and holistic approaches, and the Internet has plenty of anecdotal evidence and opinions.
In this section, we’ll look at a variety of commonly touted allergy treatments that might bring relief to CPAP machine users.
Like any medical tips you find online, we recommend you consult a medical professional before trying these to avoid any potential downsides for your specific health factors, environment, and symptoms.
Saline Nasal Irrigation, Nasal Rinsing, or Neti Pots
Saline nasal irrigation, which involves flushing the nasal passages with a saline solution, can help sleep apnea patients by reducing nasal congestion, decreasing inflammation, and clearing mucus, allergens, and irritants.
Improved nasal airflow and reduced inflammation can alleviate sleep apnea symptoms, particularly for those with obstruction caused by nasal congestion.
Before incorporating saline nasal irrigation into your routine, please consult your healthcare provider to ensure it is appropriate for your specific situation and learn the proper technique.
Using the correct method and maintaining a clean and sterile device is essential to prevent introducing any additional irritants or infections.
Consuming Local Honey
Local honey has been suggested as a potential natural remedy for seasonal allergies.
The theory is that local honey contains small amounts of pollen from the surrounding environment.
By ingesting this honey regularly, individuals may be exposed to these allergens in a low and controlled dose, which could help their immune system build tolerance over time.

As a result, seasonal allergy symptoms like nasal congestion and inflammation might be reduced, improving breathing during sleep and alleviating sleep apnea symptoms related to nasal blockages.
However, we must point out that scientific evidence supporting the effectiveness of local honey as a treatment for seasonal allergies is limited and inconclusive.
For sleep apnea patients with seasonal allergies, consult a healthcare provider to discuss if this approach might benefit you before relying upon it as a treatment option.
Eucalyptus Oil
Eucalyptus oil, derived from the leaves of the eucalyptus tree, is often touted for its anti-inflammatory, analgesic, and decongestant properties.
For people with allergies and sleep apnea, using eucalyptus oil can potentially help alleviate nasal congestion and inflammation by promoting the opening of nasal passages and easing mucus buildup.
As a result, improved breathing during sleep reduces sleep apnea symptoms and contributes to better overall sleep quality.
Using eucalyptus oil safely and according to the recommended guidelines is vital, as improper use can cause adverse effects.
The oil can be inhaled through a diffuser or applied topically when diluted with carrier oils.
However, it should never be ingested or applied undiluted to the skin.
Before incorporating eucalyptus oil into your routine, please consult your healthcare provider to ensure it is appropriate for your situation and discuss potential interactions with other medications or treatments.
While eucalyptus oil might provide some relief, it is essential to continue with evidence-based treatments, such as PAP therapy or lifestyle changes for sleep apnea and seasonal allergies, as your healthcare provider advises.
Conclusion
Allergies and sleep apnea can be a complex combination, but understanding their relationship is crucial for effective treatment.
Nasal allergies can worsen sleep apnea symptoms, but there are ways to alleviate these effects.
Lifestyle changes, such as reducing allergens in your living and workspaces, showering before sleep, and removing pets from your bedroom, can help improve symptoms and sleep quality.
Medical treatments such as taking antihistamines or decongestants, starting allergen immunotherapy, or using PAP therapy can help reduce the signs of allergies and sleep apnea.
While the evidence is anecdotal at best, several home remedies suggested for allergy symptoms might also bring results.
If you or someone you love suffers from sleep apnea, then CPAP Supply has the solution. We offer new and refurbished CPAP machines that provide an effective and affordable way to treat this common disorder. With our top-of-the-line products and expert customer service, we can help improve your quality of life with a reliable therapy system explicitly tailored to your needs. Don’t wait any longer—take control of your health today by getting the relief you deserve!