Covering the types and known causes of sleep apnea to help you identify if this potentially serious sleep order is something you should worry about.
The American Sleep Apnea Association estimates that as much as 80% of existing cases of Obstructive Sleep Apnea each year go undiagnosed.
This means untold people are dealing with the effects of sleep apnea without any knowledge that treatment and management options are available to greatly restore sleep quality and reduce the risk of a range of other ailments, including hypertension, stroke, and depression.
In this introductory guide, we’ll explore the essentials of sleep apnea. By the time you’ve finished reading, you’ll know about the common types of sleep apnea, symptoms to be aware of, and potential next steps to confirm or deny the possibility of sleep apnea for yourself or someone you love.
DISCLAIMER: This article is intended to serve as a general information guide about this critical medical topic. It is in no way to be considered professional medical advice. If you suspect you or someone you know is experiencing sleep apnea symptoms, consult with a medical professional for an official diagnosis.
What is Sleep Apnea?
Sleep apnea is a sleep disorder that results in intermittent breathing during the typical sleep cycle. Exactly how this happens depends on which type of sleep apnea is occurring.
Regardless of the type, this is a potentially serious condition that can shorten life expectancy and reduce the quality of life for people with sleep apnea.
The three major types of sleep apnea include:
Obstructive sleep apnea (OSA)
As the name suggests, obstructive sleep apnea occurs when airways are blocked, preventing breathing temporarily. This typically happens when throat muscles relax, allowing the soft palate, sidewalls of the throat, and the tongue (or any combination of) to shift in a way that restricts airflow.
Central sleep apnea (CSA):
This form of sleep apnea is less common. Central sleep apnea occurs when the brain fails to send signals to your breathing muscles to maintain a steady respiratory rate.
Complex sleep apnea syndrome:
Also known as treatment-emergent central sleep apnea or mixed sleep apnea, this isn’t a separate form of sleep apnea but a combination of obstructive and central sleep apnea. The complexity of this form can make it harder to treat and cause symptoms to manifest with greater severity.
Potential Complications & Comorbidities of Untreated Sleep Apnea
Sleep apnea itself probably sounds scary. The complications it causes are often just as serious — if not more severe — than the sleep disorder itself.
Common complications or comorbidities of people with sleep apnea include:
- Recurring heart problems: Sleep apnea increases risk factors for a range of serious heart conditions, including recurrent heart attacks, stroke, and atrial fibrillation.
- Metabolic Syndrome: Often linked with a higher risk of heart disease, metabolic syndrome symptoms include hypertension (high blood pressure), elevated cholesterol levels, hyperglycemia (high blood sugar) and increased waist circumference.
- General fatigue: When your body senses a drop in oxygen levels, it will often jolt you awake just long enough to restore airflow. While you might not remember it happening, this can happen multiple times per hour. As you might suspect, this can lead to fatigue, sluggishness, headaches, and weakness the following day.
- High blood pressure (hypertension): Caused by intermittent and sudden drops in blood oxygen levels, high blood pressure is common alongside sleep apnea.
- Type 2 Diabetes: Even mild cases of sleep apnea can result in increased risk for insulin resistance and Type 2 diabetes.
- Decreased liver function: Liver function abnormalities and nonalcoholic fatty liver disease are more common for sleep apnea patients.
- Medical treatment complications: Obstructive sleep apnea, in particular, can create elevated risk when sedated or anesthetized and laying on your back.
Of course, there are also the less medical but no-less-relevant issues caused as well.
Sleep apnea often leads to tossing and turning, snoring, gasping, coughing, and other things that won’t just interrupt your sleep but can impact your partner and family members as well.
What are the Risk Factors for Sleep Apnea?
Virtually anyone can suffer from sleep apnea — including children and teens. However, certain factors can elevate your chance of developing sleep apnea. These differ based on the type of sleep apnea in question.
Obstructive Sleep Apnea Risk Factors
- Alcohol, sedative, or tranquillizer use: Any substance that relaxes your throat muscles increases obstructive sleep apnea probability.
- Smoking: According to Mayo Clinic, smokers are three times more likely to develop obstructive sleep apnea than non-smokers due to increased inflammation and fluid build-up in upper airways.
- Obesity: Fat deposits can distort or block your upper airways, obstructing airways during sleep. This is one of the leading risk factors today.
- Ageing: Sleep apnea is more common in older populations than younger ones.
- Biological sex: Males have an increased chance of sleep apnea. However, post-menopausal women also see an elevated risk.
- Genetics and family history: If sleep apnea runs in your family, your chances are elevated as well. Physical traits, such as wide neck circumferences and narrow airways, can also elevate your risk.
- Tonsillitis or enlarged adenoids: Swelling of either of these can result in airway obstruction. Due to the smaller size of their throats, this is a common cause of sleep apnea in younger children.
- Nasal congestion: Whether you have anatomical issues that make it difficult to breathe through your nose or suffer from seasonal allergies or other ailments, nasal congestion can increase the risk of obstructive sleep apnea.
Central Sleep Apnea Risk Factors
- Ageing: Middle-aged and older persons are at greater risk of central sleep apnea than children and teens.
- Congestive heart failure: Heart disorders all elevate the risk of central sleep apnea, but congestive heart failure appears to have an increased impact on sleep apnea occurrence and serious complications.
- Biological sex: Women experience central sleep apnea at lower rates than men.
- Stroke: Suffering from a stroke increases both central and treatment-emergent central sleep apnea risk.
- Narcotic pain medication use: Opioids are known to increase the risk of sleep apnea. This includes long-acting opioids such as methadone.
Common Symptoms of Sleep Apnea
If you experience any of the following symptoms, it might be time to consult with your doctor about your sleep apnea risk. Today’s diagnosis processes are straightforward, and treatment options are both accessible and varied to help you find an ideal balance of cost, comfort, and symptom management.
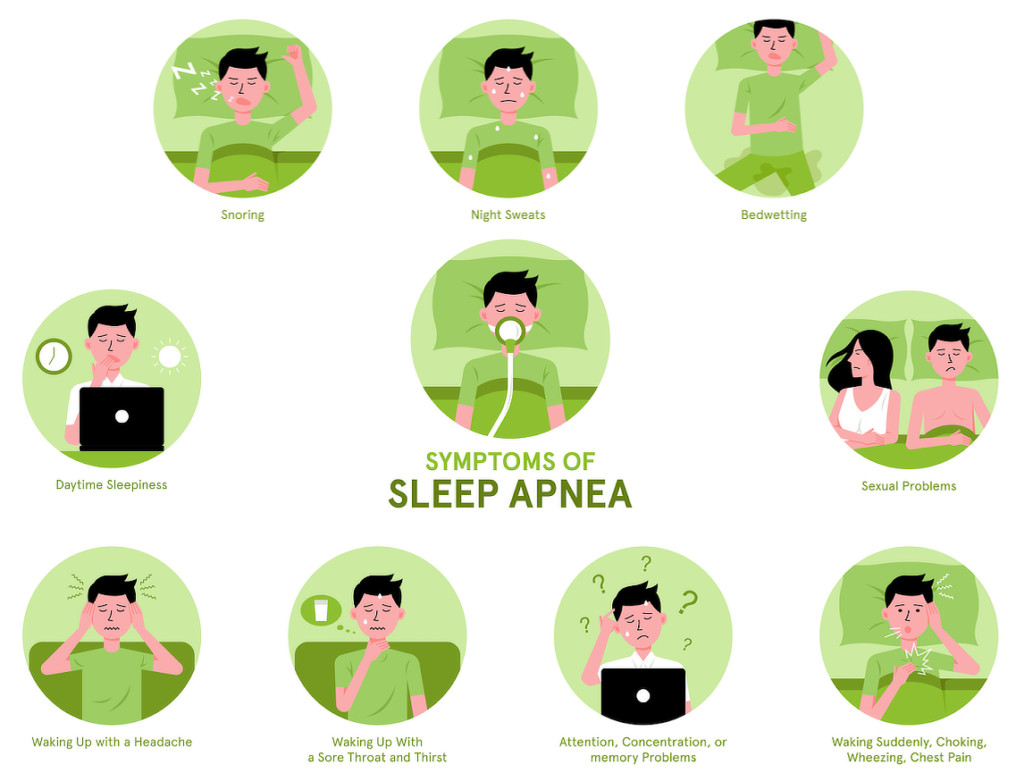
- Morning headache
- Gasping breaths during sleep
- Loud snoring
- Periodic breathing pauses during sleep — often followed by a loud snore, gasp, or jolting motion
- Sleep disorders, such as insomnia
- Daytime drowsiness or fatigue
- Difficulty focusing (both mentally or visually)
- General mood changes including irritability, aggression, or depression
- Dry mouth
Note: In many cases, spouses are the first to detect common symptoms in their partners since the person with sleep apnea isn’t aware of them. If any of these sounds like someone you know, it could also be time to consult with a primary care provider.
Common Questions about Sleep Apnea
1. Is untreated sleep apnea fatal?
As discussed in this blog post from Harvard Health Publishing, sleep apnea itself is rarely fatal. The body naturally attempts to wake up the sleeper when they stop breathing and after a snort or jolt, they’re happily breathing again.
However, that doesn’t mean that the brief periods of oxygen deprivation, the extended lack of quality sleep, the high blood pressure, and all of the various health problems that follow obstructive or central sleep apnea don’t seriously shorten life expectancy.
For example, according to Cleveland Clinic, sleep apnea occurs in roughly 50% of people with heart failure or atrial fibrillation. So while it might rarely be a primary cause of death, it is certainly a factor in an untold number of deaths each year.
2. Can children suffer from sleep apnea?
While this sleep disorder is more prevalent in older adults — particularly males — that doesn’t mean that infants, children, or teens are immune.
Risk factors for sleep apnea in young people include thick necks, nasal obstructions, excessive weight, enlarged tonsils, small jaws with overbites, and low-hanging soft palates.
If you suspect your child is experiencing sleep apnea symptoms, consult with your family doctor or pediatrician for recommended next steps.
3. What should I do if I suspect I (or someone I know) has sleep apnea?
With the amount of information at everyone’s fingertips today, it’s easy to search up endless medical information that might or might not be accurate, lead to increased stress, or even cause you to try unproven and possibly risky treatments for something that might not even exist.
As such, if you have any suspicion that sleep apnea may be causing issues for you or someone you know, schedule an appointment with your primary care provider. By looking at your health information, family history, and running a few simple tests, your doctor can ofter see if your sleep apnea concerns are warranted and recommend next steps such as a sleep study or continuous positive airway pressure (CPAP) machine usage.
4. Is there a cure for sleep apnea?
Unfortunately, there are no guaranteed ways to cure sleep apnea — particularly central sleep apnea. However, with proper treatment and possibly a few modifications to your lifestyle and daily habits, it is very possible to restore your quality of sleep and quality of life.
For obstructive sleep apnea, doctors will often recommend a combination of weight loss through diet and exercise alongside the use of a continuous positive airway pressure (CPAP), bilevel positive airway pressure (BPAP), or automatic positive airway pressure (APAP) machine.
Advances in machine technologies have reduced the overall cost of treatment, made machines more convenient to use, and provide greater comfort (and therefore better sleep) for those suffering from untreated sleep apnea.
There are also surgical options available. However, they all tend to be intrusive. As such, they’re typically reserved for situations in which PAP therapies and other approaches fail to improve CSA or OSA symptoms.
5. Does sleep apnea diagnosis require medical specialists?
In most cases, your primary doctor will start the diagnosis process. While there are some home sleep tests available, portable monitors can sometimes miss important indicators.
As such, referral to a sleep specialist for nocturnal polysomnography (sometimes called a sleep study) is common.
Depending on the results of these tests, you might also see an ear, nose, and throat specialist (otolaryngologist), a nervous system specialist (neurologist) or a heart specialist (cardiologist.)
6. Do mouthpieces for sleep apnea work?
Oral appliances are a common alternative to traditional PAP therapies for people with obstructive sleep apnea. However, effectiveness is often hard to predict and will depend on a variety of factors, including the severity of your sleep apnea symptoms and the design of the oral appliance.
The most effective mouthpieces are typically designed in partnership with a trained dental specialist. Over-the-counter or mass-produced models may not provide effective relief.
Key Takeaways
- Because sleep apnea symptoms may appear as minor inconveniences or occur when the person is sleeping, professionals estimate that a considerable percentage of sleep apnea cases go undiagnosed every year.
- Sleep apnea is a serious condition with the potential to shorten life expectancy and diminish quality of life.
- Sleep apnea can effect people of all ages.
- Sleep apnea often coexists with other serious medical conditions and complications, further increasing the risk of significant adverse health events.
- Obstructive sleep apnea is the most common form, followed by central sleep apnea and treatment-emergent central apnea syndrome.
- Risk factors for sleep apnea will differ based on the type of sleep apnea.
- Common symptoms include daytime fatigue, morning headache, loud snoring, dry mouth, difficulty focusing, and mood changes.
As Canada’s leading online CPAP supply store in customer satisfaction, CPAPSupply.ca is proud of our ability to help improve the lives of sleep apnea sufferers across the country. We’re available seven days a week to discuss your exact needs and help to find high-quality options from leading brands such as ResMed, Phillips Respironics, HDM, and more to help you not simply sleep better but live a better life as well. Contact us today to discuss our selection of CPAP machines, CPAP masks, CPAP accessories, and mask parts.
References:
- The Mayo Clinic: Sleep Apnea Symptoms & Causes
- The Mayo Clinic: Obstructive Sleep Apnea Symptoms & Causes
- Sleep Foundation: Sleep Apnea: What It Is, Its Risk Factors, Its Health Impacts, and How It Can Be Treated
- National Institutes of Health National Heart, Lung, and Blood Institute: Sleep Apnea
- Medical News Today: What You Need To Know About Sleep Apnea
- MedLine Plus: Sleep Apnea
- Cleveland Clinic: Health Library: Sleep Apnea
- American Sleep Apnea Association: Sleep Apnea is a Dangerous Condition
- Healthline: Obstructive Sleep Apnea
- American Academy of Sleep Medicine: Obstructive Sleep Apnea
- Wikipedia: Sleep Apnea
- Everyday Health: What Is Sleep Apnea? Symptoms, Causes, Diagnosis, Treatment, and Prevention
- I Need Better Sleep: Sleep Apnea Statistics
- Annals of Thoracic Medicine: A Systematic Review on Prevalence and Risk Factors Associated With Treatment-Emergent Central Sleep Apnea
- Harvard Health Blog: Snored to Death: The Symptoms and Dangers of Untreated Sleep Apnea
- WebMD: Sleep Apnea May Be Deadly

